Highlight
- FFR-guided complete revascularization significantly reduces the composite risk of death, nonfatal myocardial infarction, repeat revascularizations, and stroke compared to culprit-only PCI in NSTEMI patients with multivessel disease.
- The benefit is largely driven by a notable reduction in repeat revascularization procedures over 1 year.
- Complete revascularization was safely performed during the index procedure without increase in major adverse events despite longer procedure time and higher contrast use.
- These findings support FFR-guided complete revascularization as a strategic standard in managing NSTEMI with multivessel coronary artery disease.
Introduction
Multivessel coronary artery disease (CAD) is present in approximately half of patients presenting with non–ST-elevation myocardial infarction (NSTEMI), a subgroup historically associated with challenging management and variable outcomes. While multiple randomized trials have firmly established the benefit of complete revascularization in ST-elevation myocardial infarction (STEMI), clear evidence in NSTEMI patients remains limited, with most data deriving from observational or mixed acute coronary syndrome cohorts. Treatment strategies have varied between culprit-only revascularization and staged or immediate complete revascularization, with uncertainty over optimal lesion assessment and timing for intervention on nonculprit lesions.
Fractional flow reserve (FFR) offers a physiological assessment of lesion significance that has demonstrated benefit in stable CAD and STEMI, but its role in NSTEMI with multivessel disease remains under-investigated. Given that visual angiographic evaluation often overestimates lesion severity and might lead to unnecessary stenting, FFR-guided strategies may optimize revascularization decision-making. Importantly, current American and European guidelines express only modest recommendations for routine use of invasive functional assessment in NSTEMI nonculprit lesions, underscoring the need for robust randomized data.
Study Design
The South Limburg Myocardial Infarction (SLIM) trial was a prospective, multinational, randomized clinical trial conducted across 9 hospitals in Europe from June 2018 to July 2024, with final follow-up through July 2025. This investigator-initiated study enrolled adult patients (aged 18–85) presenting with NSTEMI and multivessel CAD who had successful PCI of the culprit lesion and had at least one nonculprit lesion with stenosis ≥50% amenable to revascularization.
Participants were randomized 1:1 after culprit lesion PCI to either:
1. FFR-guided complete revascularization group: immediate PCI at the index procedure on all nonculprit lesions with FFR ≤0.80, with staged PCI only in exceptional cases within the hospitalization.
2. Culprit-only revascularization group: PCI limited to the culprit lesion during the index procedure. Staged nonculprit PCI within 6 weeks was permitted based on clinical judgment.
Primary outcome was a composite of all-cause mortality, nonfatal myocardial infarction, any revascularization, and stroke at one year. Secondary endpoints included individual components, net adverse clinical events (composite of cardiac death, MI, any revascularization, stroke, and major bleeding), cardiac rehospitalization, and bleeding events. Independent adjudication was blinded to treatment assignments.
Key Findings
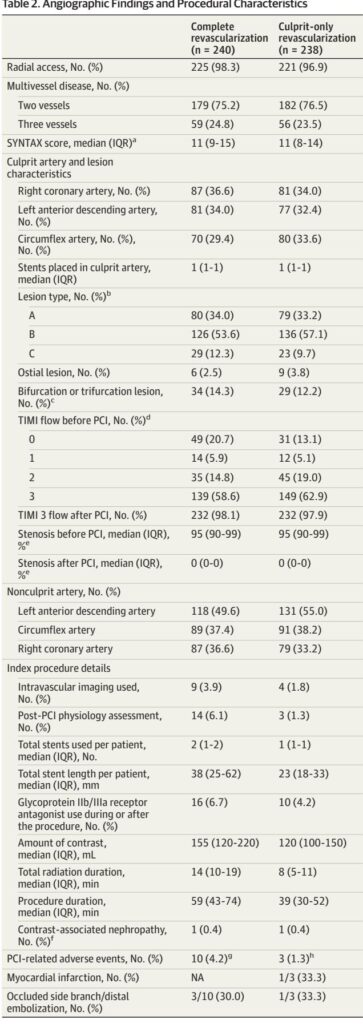
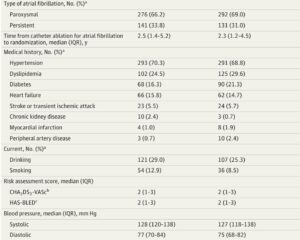
A total of 478 patients were randomized (240 to complete revascularization, 238 to culprit-only). Baseline characteristics were well-balanced except for slightly higher diabetes prevalence and BMI in the complete revascularization group. The majority had two-vessel disease, and SYNTAX scores were similar.
At 1-year follow-up, the primary composite outcome occurred in 5.5% of patients in the FFR-guided complete revascularization group versus 13.6% in the culprit-only group, translating to a hazard ratio (HR) of 0.38 (95% CI, 0.20–0.72; P=0.003). This represents a substantial relative risk reduction favoring complete revascularization.
This reduction was predominantly driven by a marked decrease in any revascularization events (3.0% vs 11.5%; HR 0.24, 95% CI 0.11–0.56; P<0.001). There was a trend toward fewer nonfatal myocardial infarctions in the complete revascularization group (2.1% vs 5.1%; HR 0.40, 95% CI, 0.14–1.15), which became statistically significant in an extended follow-up post hoc analysis (HR 0.35, 95% CI 0.13–0.97).
No significant differences were found in all-cause mortality, cardiac death, or stroke between groups. Net adverse clinical events were lower in the complete revascularization group (6.3% vs 15.3%, HR 0.39, 95% CI 0.21–0.70; P=0.002). Bleeding and safety endpoints, including stent thrombosis, were similar.
Procedurally, complete revascularization was associated with longer procedure and radiation times and higher contrast volume, though complication rates related to PCI were low and acceptable. Seven patients crossed over from culprit-only to complete intervention. Staged PCI in the culprit-only arm was performed in 13% of patients but was not counted as an event unless unplanned or beyond 6 weeks.
Subgroup analyses by diabetes status, age, sex, and GRACE risk score showed consistent benefit with no significant interaction effects.
Expert Commentary
The SLIM trial provides compelling evidence that FFR-guided complete revascularization at the index procedure improves clinical outcomes in patients with NSTEMI and multivessel disease. It extends the paradigm established in STEMI populations by confirming benefits in NSTEMI, a group with unique pathophysiology and diagnostic challenges.
The study smartly harnesses physiological assessment to mitigate overestimation of lesions inherent to angiography alone, a critical consideration given the morbidity associated with unnecessary stenting. Moreover, by performing complete revascularization during the index procedure, the trial addresses concerns of deferred ischemia and potential event risks associated with staged interventions.
Its robust randomized design and high follow-up completeness add strength, although the modest event rates and relatively short follow-up limit definitive conclusions on mortality or long-term myocardial infarction reduction. The open-label nature and allowance for staged PCI in the culprit-only group could bias results toward reduced events in the complete revascularization arm, though analyses including per-protocol and as-treated sets were concordant.
Noteworthy is that the trial focuses strictly on NSTEMI patients, complementing prior mixed-population studies (e.g., FIRE, FRAME-AMI) and aligning with current guideline directions that emphasize individualized functional lesion assessment.
Limitations include modest power for individual outcome components, incomplete data on screened but non-enrolled patients limiting external validity, and limited use of adjunct intracoronary imaging which may further refine lesion characterization in unstable plaques.
Future research should examine long-term outcomes, explore integration of intravascular imaging, and assess cost-effectiveness of FFR-guided complete revascularization strategies.
Conclusion
The SLIM trial establishes that FFR-guided complete coronary revascularization during the index procedure significantly reduces the combined incidence of death, nonfatal myocardial infarction, repeat revascularization, and stroke in patients with NSTEMI and multivessel coronary artery disease, driven chiefly by fewer repeat revascularizations. These findings support integrating physiological lesion assessment into routine practice and favor complete immediate revascularization to optimize clinical outcomes in this high-risk population.
References
Pustjens TFS, Veenstra L, Camaro C, Ruiters AW, Lux Á, Ruzsa Z, Piroth Z, Ilhan M, Vainer J, Gho B, Winkler PJC, Stein M, Theunissen RALJ, Kala P, Polad J, Berta B, Gabrio A, van Royen N, van ‘t Hof AWJ, Rasoul S. Fractional Flow Reserve-Guided Complete vs Culprit-Only Revascularization in Non-ST-Elevation Myocardial Infarction and Multivessel Disease: The SLIM Randomized Clinical Trial. JAMA. 2025 Aug 31. doi: 10.1001/jama.2025.16189. Epub ahead of print. PMID: 40886310.