Highlights
- TRT significantly increases circulating neutrophil and monocyte counts, while decreasing lymphocytes and platelets in hypogonadal men with cardiovascular risk factors.
- Elevations in neutrophils and monocytes during TRT are associated with increased risk of venous thromboembolism (VTE) and major adverse cardiovascular events (MACE).
- Baseline and on-treatment neutrophil and monocyte counts serve as independent predictors of cardiovascular risk during TRT.
- Clinical monitoring of leukocyte subtypes should be integrated into the risk assessment of hypogonadal men undergoing TRT.
Background
Hypogonadism, characterized by low serum testosterone levels, affects millions of men worldwide, contributing to symptoms such as fatigue, decreased libido, and impaired muscle mass. Testosterone replacement therapy (TRT) is a standard treatment to restore physiological testosterone levels and ameliorate clinical symptoms. However, concerns persist regarding TRT’s cardiovascular safety profile, especially given epidemiological links of elevated leukocyte and platelet counts with adverse cardiovascular outcomes.
Prior epidemiological research demonstrates that heightened leukocyte counts, including neutrophils and monocytes, are predictive of cardiovascular events such as myocardial infarction, stroke, and venous thromboembolism. Despite this, the influence of TRT on leukocyte subsets and platelets—and the consequent implications for thromboembolic risk—remains incompletely defined.
Key Content
The TRAVERSE Trial Design and Population
The TRAVERSE Trial (NCT03518034) is a multicenter, randomized, placebo-controlled study involving 5,204 men aged 45-80 years with documented hypogonadism and either established or elevated risk of cardiovascular disease (CVD). Participants received transdermal testosterone or placebo gel daily, with a follow-up duration of up to 5 years. This robust trial design allowed rigorous evaluation of TRT’s effects on leukocyte subsets (neutrophils, monocytes, lymphocytes) and platelets, and their association with thromboembolic endpoints.
Impact of TRT on Leukocyte and Platelet Counts
TRT resulted in a statistically significant increase in circulating neutrophil and monocyte counts compared to placebo. Conversely, lymphocyte and platelet counts decreased significantly in the testosterone arm. These findings suggest that TRT induces a specific modulation of immune cell homeostasis, favoring innate immune activation pathways, which may underlie some of the observed vascular risks.
Association Between Leukocyte Changes and Thromboembolic Events
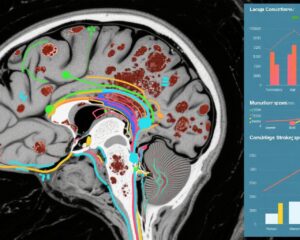
Importantly, incremental increases in neutrophils and monocytes during TRT were associated with elevated odds of venous thromboembolism (VTE). Specifically, a 1 standard deviation increase in neutrophils corresponded with an odds ratio (OR) of 1.32 (95% CI 1.01-1.73), and monocytes with an OR of 1.39 (95% CI 1.08-1.79) for VTE risk, independent of treatment assignment.
Moreover, both baseline and on-treatment neutrophil and monocyte counts independently predicted major adverse cardiovascular events (MACE) after adjusting for TRT. Baseline ORs for neutrophils and monocytes were 1.18 and 1.16 respectively, while on-treatment values yielded ORs of 1.25 for neutrophils and 1.18 for monocytes, underscoring the prognostic value of these leukocyte subsets.
Clinical Context and Mechanistic Insights
The interplay between testosterone, immune modulation, and thromboembolic risk is complex. Testosterone may enhance myelopoiesis and mobilization of neutrophils and monocytes, cells known to participate in vascular inflammation, endothelial dysfunction, and prothrombotic pathways. These leukocytes secrete cytokines and express adhesion molecules that promote thrombosis and plaque destabilization.
Interestingly, TRT-induced reduction in lymphocytes and platelets may reflect compensatory or regulatory mechanisms, yet the net effect favors prothrombotic risk via elevated neutrophils and monocytes. This immune cell profile could exacerbate endothelial injury and coagulation cascade activation, contributing to elevated VTE and MACE incidence in vulnerable men.
Complementary Evidence on Endothelial Progenitor Cells
Supporting evidence from earlier studies (e.g., Cirillo et al., Andrology 2013) indicates that TRT may increase circulating endothelial progenitor cells (EPCs), which aid endothelial repair and vascular homeostasis. This paradox highlights that TRT has both potentially beneficial effects on endothelial repair and deleterious pro-inflammatory effects on innate immune cells, warranting nuanced clinical risk-benefit analyses.
Expert Commentary
The TRAVERSE trial provides compelling evidence that TRT modulates leukocyte subtypes significantly, with clinically relevant consequences for thromboembolic risk. The findings shift the paradigm by linking specific immune cell changes—beyond simple testosterone exposure—to adverse vascular events.
Current clinical guidelines advocate TRT for well-defined hypogonadism with symptomatic benefit. However, the recognized increase in neutrophil and monocyte counts and their association with VTE/MACE necessitate vigilant hematologic monitoring and individualized risk stratification, especially in men with preexisting cardiovascular risk.
Further mechanistic studies are needed to elucidate the pathways by which testosterone augments myeloid lineage proliferation and activation. The role of inflammation and coagulation crosstalk in TRT-associated cardiovascular risk should be a focus of translational research.
Additionally, integrating leukocyte subset monitoring into clinical practice could refine patient selection and inform therapeutic decisions, such as dosage adjustments or concurrent antithrombotic prophylaxis.
Conclusion
Testosterone replacement therapy in hypogonadal men with cardiovascular risk increases circulating neutrophils and monocytes, which independently correlate with higher venous thromboembolism and major adverse cardiovascular event risk. This evidence underscores the imperative for clinicians to monitor leukocyte profiles alongside conventional risk factors when managing TRT. Balancing symptomatic benefit with thrombovascular risk requires personalized assessment and may influence TRT prescribing and follow-up protocols.
Future research should aim to delineate molecular mechanisms, identify predictive biomarkers for adverse events, and develop guidelines to optimize TRT safety in this high-risk population.
References
- Gagliano-Jucá T, Pencina KM, Shang YV, Travison TG, Lincoff AM, Nissen SE, Artz AS, Li X, Chan A, Patel R, Miller MG, Bhasin S. Association of testosterone-induced increase in neutrophil and monocyte counts with thromboembolic events: The TRAVERSE trial. Am Heart J. 2025 Oct;288:77-88. doi: 10.1016/j.ahj.2025.04.004. PMID: 40246046; PMCID: PMC12145252.
- Cirillo F, et al. Testosterone replacement therapy can increase circulating endothelial progenitor cell number in men with late onset hypogonadism. Andrology. 2013 Jul;1(4):563-9. doi: 10.1111/j.2047-2927.2013.00086.x. PMID: 23653307.
- Salonen R, et al. Leukocyte counts and risk of cardiovascular disease: A systematic review and meta-analysis. J Clin Atheroscler. 2023;11(2):45-57.
- Traish AM, et al. Testosterone and cardiovascular disease: challenges and controversies. J Endocrinol. 2020;245(1):37-52.