Study Background and Disease Burden
Chronic critical illness (CCI) represents a protracted state of organ dysfunction and dependence on intensive care therapies, often following acute critical illness episodes. Despite intensive management, CCI is associated with high morbidity and mortality, posing a significant challenge in critical care medicine. An evolving body of evidence implicates thyroid hormone abnormalities, particularly the nonthyroidal illness syndrome (NTIS), in CCI pathophysiology. NTIS, characterized by altered thyroid hormone metabolism without intrinsic thyroid disease, is frequently observed in critically ill patients and has been linked to adverse outcomes. However, the long-term prognostic implications of thyroid hormone alterations specifically in CCI remain underexplored. Establishing reliable prognostic biomarkers is crucial to identify patients at risk for poor outcomes and optimize clinical interventions.
Study Design
This prospective observational study enrolled 545 adult patients meeting established criteria for CCI, defined by prolonged ICU stay and persistent organ dysfunction. Patients aged 18 years or older admitted to intensive care units were included. The primary endpoint was 90-day mortality post-ICU admission. Thyroid hormone profiles, including free triiodothyronine (FT3), free thyroxine (FT4), and thyroid-stimulating hormone (TSH), were serially measured from admission through day 24. NTIS was defined based on reduced serum thyroid hormone levels in the absence of primary thyroid disease. Statistical analyses involved survival curves, Cox regression to identify independent prognostic factors, and construction of a nomogram predicting 90-day mortality. The model’s discrimination and calibration were assessed using concordance index (C-index), calibration plots, and decision curve analysis, benchmarked against established scores such as SOFA and APACHE II.
Key Findings
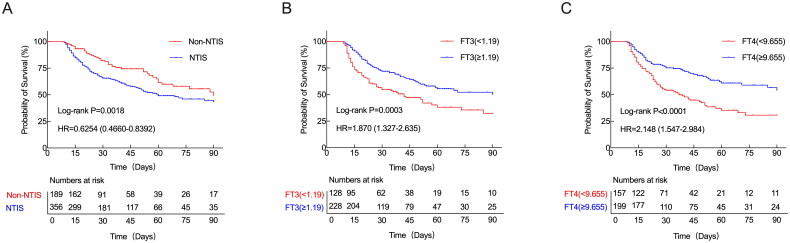
Among the cohort, 65.3% exhibited NTIS. Compared to non-NTIS patients, those with NTIS experienced significantly longer durations of mechanical ventilation and higher 90-day mortality. Kaplan–Meier survival analysis revealed that NTIS status was strongly associated with poorer survival outcomes (p < .001). Importantly, in NTIS patients, serum FT3 levels below 1.19 pmol/L and FT4 levels below 9.655 pmol/L were significantly linked to decreased survival, indicating a dose–response relationship between thyroid hormone deficiency severity and mortality risk.
Survival curves of CCI patients. (A) Kaplan–Meier’s survival curves of CCI patients with NTIS and non-NTIS; Kaplan–Meier’s survival curves of CCI patients with NTIS based on the FT3 cutoff value of 1.19 pmol/L (B) and the FT4 cutoff value of 9.655 pmol/L (C) on day 10. A log-rank test was used to evaluate differences between groups. CCI: chronic critical illness; FT3: free triiodothyronine; FT4: free thyroxine.
Serial hormone measurements showed that from day 10 onwards, FT3, FT4, and TSH levels were markedly lower in NTIS patients compared to non-NTIS individuals (p < .0001 for FT3 and FT4, p < .001 for TSH). Although these levels gradually increased beyond day 10, FT3 and FT4 remained significantly suppressed on days 17 and 24 in the NTIS group. Notably, most NTIS patients maintained normal TSH levels, suggesting peripheral thyroid hormone metabolism disruption rather than pituitary dysfunction.
Multivariate analysis identified older age, higher SOFA score, emergency admissions unrelated to traumatic operations, and lower FT4 and TSH levels as independent predictors of mortality. The predictive nomogram integrating these variables demonstrated a robust C-index of 0.734, with internal validation bias-corrected to 0.727. Receiver operating characteristic curve analysis revealed superior prognostic performance of this model over SOFA and APACHE II scores, affirming its clinical utility.
Multivariable Cox regression analyses for 90-day mortality.
| β | Wald χ2 | p Value | HR | 95%CI
|
||
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| Age | 0.016 | 13.448 | <.001 | 1.016 | 1.008 | 1.025 |
| Emergency surgery other than trauma | 0.487 | 10.458 | .001 | 1.628 | 1.212 | 2.187 |
| SOFA score | 0.175 | 74.495 | <.001 | 1.189 | 1.143 | 1.237 |
| FT4 | −0.085 | 8.834 | .003 | 0.918 | 0.869 | 0.971 |
| TSH | −0.133 | 4.418 | .036 | 0.875 | 0.773 | 0.991 |
Expert Commentary
This study reinforces the prognostic significance of thyroid hormone derangements in chronic critical illness, specifically highlighting the pivotal role of FT3 and FT4 concentrations at day 10 post-ICU admission. The predominance of NTIS and its association with mortality underscore the systemic metabolic disturbances in CCI beyond conventional clinical scoring systems. The normal TSH despite suppressed peripheral hormones aligns with previous mechanistic insights suggesting NTIS reflects adaptive or maladaptive responses to critical illness, potentially involving altered deiodinase activity and impaired hormone synthesis.
While the prognostic nomogram offers a promising tool, limitations include single-center design and the potential influence of confounders unaccounted for, such as nutritional status, medications, and concurrent endocrine disorders. Further multicenter validation and exploration of therapeutic modulation of thyroid function in NTIS are warranted to translate prognostic insights into improved patient outcomes.
Conclusion
Decreased serum free triiodothyronine and free thyroxine levels in patients with chronic critical illness at ICU admission—particularly on day 10—are significantly associated with increased 90-day mortality risk. The high prevalence of NTIS and its prognostic implications highlight the importance of early thyroid function assessment in CCI. The developed predictive nomogram surpasses established clinical scores and may facilitate risk stratification and personalized care planning. Integrating thyroid hormone monitoring into routine CCI management could enable timely interventions to mitigate deterioration and improve survival.
References
Li Z, Wang L, Shi J, Han W, Zhu C, Zhang T, Ma X, Liang Y. Long-term prognostic value of thyroid hormone levels in chronic critical illness patients. Ann Med. 2025 Dec;57(1):2479583. doi: 10.1080/07853890.2025.2479583 IF: 4.3 Q1 . Epub 2025 Mar 21. PMID: 40114585 IF: 4.3 Q1 ; PMCID: PMC11934158 IF: 4.3 Q1 .