The 7th Experts in Stone Disease (ESD) Conference (Bucharest, 2025) produced a practical, multidisciplinary consensus on urinary stone management that synthesizes recent pathophysiologic insights, pharmacologic advances and rapid technological changes in endourology. The ESD 2025 statements complement contemporary society guidance (notably the European Association of Urology 2025 update) by focusing on: (1) why stones cause kidney damage, (2) a stronger emphasis on individualized metabolic and morpho‑compositional diagnostics, (3) prevention with both established and emerging agents, and (4) safe, evidence‑informed use of novel endoscopic tools (suction sheaths, DISS, new lasers and ultra‑thin disposable flexible ureteroscopes).
Why now? Two converging trends made this consensus timely: modern research reframing lithogenesis as a multi‑hit process involving inflammation and renal epithelial responses, and rapid commercialization of new endourologic devices (high‑power lasers, thulium fiber lasers, navigable suction access sheaths, disposable ultra‑slim fURS). ESD 2025 aims to help clinicians translate these advances into safer, more cost‑effective care.
New Guideline Highlights — Key Takeaways
– Universal baseline evaluation: stone analysis plus basic metabolic screen for every stone former; targeted 24‑hour urine testing for high‑risk groups.
– Stone morpho‑compositional analysis recommended routinely (stereoscopic microscopy + SEM‑EDS ± FTIR) to reconstruct etiologies and guide therapy.
– Prevention: potassium citrate remains first‑line for hypocitraturia/uric acid/cystine stones; emerging adjuncts include phytate (InsP6) for calcium stones and theobromine for uric acid crystallization—both supported by mechanistic and early clinical data but considered adjunctive/expert opinion pending large RCTs.
– Infectious (struvite) stones: complete surgical clearance, infection control, urinary acidification (e.g., L‑methionine) and metabolic re‑evaluation after sterility.
– Interventional strategy: RIRS with suction adjuncts (DISS, FANS‑UAS) and ultra‑thin disposable scopes is expanding indications, but PCNL remains preferred for large burden (>20 mm) depending on anatomy and device availability.
– Safety focus: intrarenal temperature and pressure control are essential during laser lithotripsy; limiting settings, ensuring irrigation/suction and real‑time pressure monitoring reduce injury and infection risk.
– Practical perioperative guidance for antithrombotic management and radiation exposure (ALARA) updated to reflect contemporary practice.
Updated Recommendations and Key Changes from Prior Practice
ESD 2025 does not replace formal guideline bodies but provides expert consensus on topics not fully covered elsewhere. Major updates vs older practice include:
– Pathogenesis: stronger emphasis on inflammation/oxidative stress and the role of renal epithelial responses (multi‑hit model) — implications for anti‑inflammatory or antioxidative strategies under study. (Evidence: Khan et al., Nat Rev Nephrol 2021; Rodgers 2017.)
– Diagnostics: routine morpho‑compositional stone analysis (StM + SEM‑EDS ± FTIR) rather than chemistry/IR alone — graded as Expert Consensus (EC) with growing observational support. (Daudon et al. 2016; Costa‑Bauzá 2023.)
– Endourology: acceptance of suction‑enabled RIRS (DISS, FANS‑UAS) and ultra‑thin disposable fURS for broader indications — EC with growing randomized/real‑world data (Zhu et al., EClinicalMedicine 2024; Gauhar et al., Eur Urol Focus 2024).
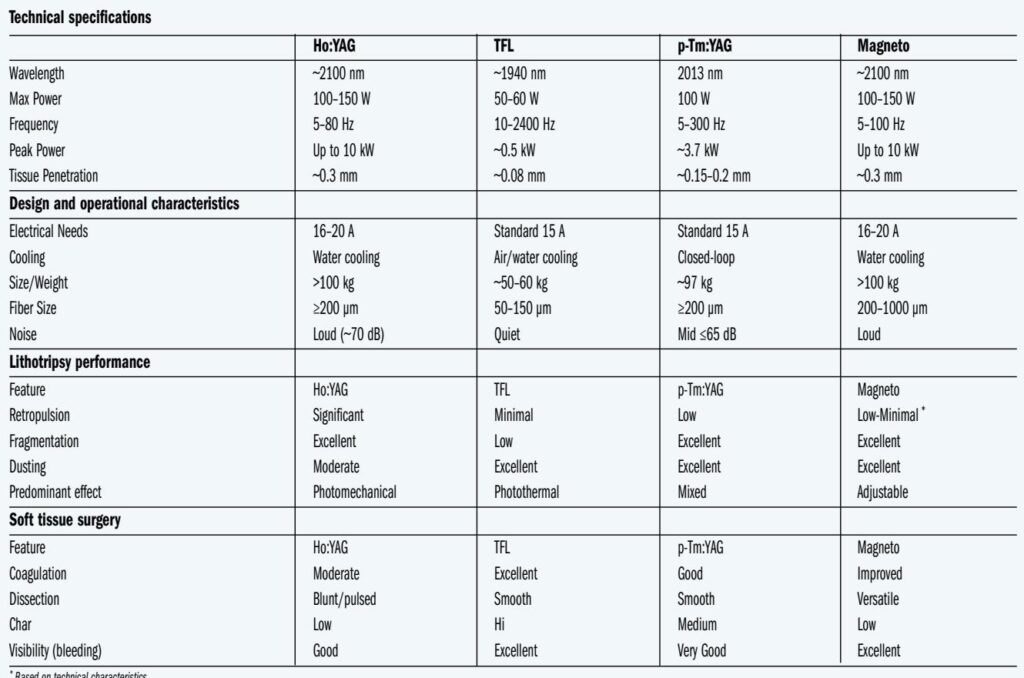
– Lasers: balanced guidance acknowledging advantages of TFL and pulse‑modulated HP Ho:YAG but adding safety caveat on heat and pressure — new recommendation to actively monitor/limit thermal exposure. (Peteinaris et al. 2023; Pauchard et al. 2022.)
– SWL: explicitly more selective use; RIRS/PCNL preferred for many cases previously managed by SWL.
Evidence grading used in this consensus: Strongly Recommended (SR — consistent high‑quality evidence or guideline alignment), Recommended (R — moderate evidence), Expert Consensus (EC — limited or emerging data; panel opinion).
Topic‑by‑Topic Recommendations
– Diagnostic workup
– All stone formers: mandatory stone analysis (morpho‑compositional when available), basic blood biochemistry (creatinine, electrolytes, calcium, phosphate, bicarbonate, PTH, vitamin D when indicated) and spot urine (pH, sediment, culture). (SR / aligns with IAU 2022 and EAU 2025.)
– High‑risk patients — children, recurrent stone formers, early age of onset, bilateral stones, staghorn, solitary kidney, nephrocalcinosis — obtain 24‑hour urine for calcium, oxalate, citrate, uric acid, sodium, magnesium, volume and protein; repeat 8–12 weeks after starting prevention. (SR)
– Imaging: non‑contrast low‑dose CT remains standard for acute assessment; ultrasound acceptable for follow‑up when radiation reduction desired. (R)
– Stone analysis
– Use morpho‑compositional approach routinely when available: StM → SEM‑EDS → FTIR for complex/drug‑induced stones. Benefits: reveals nucleation sites, mixed components, and patterns (Randall’s plaque, plugs) that guide diagnosis and therapy. (R/EC)
– Medical prevention and dietary measures
– Hydration: target urine output ≥2.0–2.5 L/day (SR).
– Diet: maintain normal dietary calcium (avoid low calcium), reduce sodium and excessive animal protein, moderate oxalate foods, increase dietary citrate (citrus fruits). (SR)
– Potassium citrate: first‑line for hypocitraturia and uric acid stones; monitor serum K+ and urine pH (target urine pH 6.0–6.5 for uric acid stones). (SR)
– Thiazide diuretics: for hypercalciuria after secondary causes addressed; monitor metabolic side effects and potassium. (R)
– Phytate (InsP6): promising inhibitor of calcium crystal formation; clinical use considered adjunctive in select patients (EC) with early trial data and epidemiologic support (Curhan et al. cohorts). (EC)
– Theobromine: experimental/early clinical support for preventing uric acid crystallization; consider as adjunct to lowered citrate doses to avoid over‑alkalinization (EC).
– Special metabolic conditions
– Struvite stones: require complete surgical clearance, targeted antibiotics (culture guided), urinary acidification (L‑methionine) to pH 20 mm or complex staghorn stones. (SR)
– PCNL: individualized choice of prone vs supine and standard vs mini‑PCNL based on stone burden, anatomy and surgeon experience. Use ultrasound guidance to reduce radiation where expertise exists. (R)
– RIRS and suction adjuncts: RIRS indications expanded; use suction UAS (FANS‑UAS), DISS or aspirating sheaths when available to lower IRP and temperature, improve vision and increase stone‑free rates—especially for larger stones or infected/turbid urine. (R/EC)
– Lasers: choose device by case—TFL excels at dusting/smaller stones; HP Ho:YAG (pulse‑modulated) offers fragmentation versatility. Monitor settings and limit continuous high‑power exposure; maintain irrigation/suction to control heat. (R)
– Disposable ultra‑slim fURS: appropriate for select patients (pediatric, anatomically difficult, avoid pre‑stenting); weigh cost and environmental tradeoffs. (EC)
– Intraoperative safety: pressure and thermal control
– Intrarenal pressure (IRP): maintain IRP <20–30 cm H2O when possible; avoid sustained spikes to reduce pyelovenous backflow and infection risk. Use suction sheaths and monitor when devices available. (R)
– Temperature: avoid prolonged tissue exposure to temperatures above thresholds associated with cellular injury (experimental reports highlight risk at 43°C with prolonged exposure). Practical measures: intermittent lasing, lower energy/frequency settings for dusting, optimize irrigation and suction. (R/EC)
– Perioperative antithrombotic management
– Strategy individualized by thrombosis vs bleeding risk: generally stop DOACs 48–72 hours preoperatively (depending on renal function) without routine bridging; stop warfarin 5 days preoperatively with INR target <1.5; continue aspirin for many URS procedures but stop P2Y12 agents 5–7 days if possible. Multidisciplinary consultation for high‑risk patients. (SR — aligns with Douketis et al., NEJM 2015 and EAU 2024 guidance)
– Complication reporting and follow‑up
– Use standardized classification (Clavien‑Dindo) for reporting complications but recognize limitations; collect perioperative metrics including IRP/temperature metrics where possible. (R)
– Follow up: imaging and metabolic reassessment individualized; 24‑hour urine repeat 8–12 weeks after preventive therapy initiation and then annually if stable. (R)
Practical Algorithm (concise)
1. First stone episode: stone analysis, serum chemistries, urine pH/sediment/culture, counsel on hydration/diet. (SR)
2. High‑risk or recurrent: 24‑h urine, consider morpho‑compositional stone analysis, specialist referral. (SR)
3. Acute obstructing ureteral stone with infection/sepsis: urgent decompression (stent or nephrostomy) + antibiotics. (SR)
4. Elective definitive therapy chosen by size/location/anatomy: SWL for selected <20 mm renal or 20 mm/complex stones. (SR/R)
5. Prevention: start lifestyle measures + potassium citrate or other targeted therapy guided by metabolic results. (SR)
Expert Commentary, Controversies and Research Needs
– Expanding RIRS vs PCNL: ESD panel acknowledged growing evidence that suction‑enabled RIRS with FANS‑UAS may approach mini‑PCNL outcomes for 2–3 cm stones in selected centers (Chen et al. 2024; Zhu et al. 2024). Experts caution generalizability: long‑term reintervention and cost comparisons require more RCTs.
– Thermal/pressure safety thresholds: animal and benchtop data indicate harm potential with modern lasers at high settings. Experts recommend conservative intraoperative settings and routine use of suction/irrigation rather than relying solely on lithotripsy speed. Prospective human safety data are needed.
– Phytate and theobromine: promising biologic plausibility and early data but evidence remains insufficient for broad endorsement—experts favor continued clinical trials before widespread adoption.
– Single‑use devices and sustainability: consensus recognizes clinical advantages (infection control, no repair downtime) but raises cost and environmental concerns. Centers should audit outcomes and costs; reprocessing or reuse policies need strict governance if pursued.
– Standardizing complication reporting: a urology‑specific, granular system was recommended to better capture cumulative morbidity beyond the highest Clavien grade.
Practical Implications for Daily Practice
– Diagnostics: prioritize stone retrieval and morpho‑compositional analysis when possible — the stone is often the best historical record of etiologic events.
– Prevention: invest in patient education tools (smartphone apps, home pH meters) to improve adherence—ESD highlighted validated apps (myLit‑Control) and home pH monitoring as useful adjuncts. (R)
– Endourology programs: incorporate IRP/temperature awareness into protocols; consider adopting suction‑enabled sheaths and invest in staff training for ultrasound‑guided access to reduce radiation exposure.
– Antithrombotic and infection protocols: maintain institutional multidisciplinary pathways to balance bleeding and thrombotic risks and minimize urosepsis.
– Cost and sustainability: measure reintervention rates and device costs locally; decisions on disposables vs reusable devices should include environmental and long‑term economic modeling.
Fictional vignette: applying ESD 2025 in clinic
John, a 48‑year‑old man, presents with a first symptomatic episode of flank pain and a 9 mm lower‑pole calcium oxalate stone on low‑dose CT. Urine pH 5.5, urinalysis sterile. Stone retrieved during RIRS. ESD‑guided plan:
– Send stone for morpho‑compositional analysis (StM + SEM‑EDS) and order baseline labs (Ca, P, creatinine, bicarbonate, PTH) and advise 2.5 L/day fluid intake and dietary sodium moderation. (SR)
– Because this is first episode, no immediate 24‑hour urine is mandatory, but if morpho analysis or clinical context suggests metabolic abnormality or recurrence occurs, arrange 24‑h urine. (R)
– If analysis shows hypocitraturia, start potassium citrate and provide home pH monitoring with app support to target urine pH and adherence. (SR)
– Counsel on warning signs for infection or obstruction and schedule follow‑up imaging at 4–12 weeks per local protocols. (R)
References (selected authoritative sources)
– Papatsoris A, Geavlete B, Radavoi GD, et al. Management of urinary stones by experts in stone disease (ESD 2025). Arch Ital Urol Androl. 2025;97(2):14085.
– Skolarikos A, Geraghty R, Somani B, et al. European Association of Urology Guidelines on the Diagnosis and Treatment of Urolithiasis. Eur Urol. 2025.
– Zeng G, Zhu W, Robertson WG, et al. International Alliance of Urolithiasis (IAU) guidelines on the metabolic evaluation and medical management of urolithiasis. Urolithiasis. 2022;51:4.
– Daudon M, Dessombz A, Frochot V, et al. Comprehensive morpho‑constitutional analysis of urinary stones improves etiological diagnosis and therapeutic strategy of nephrolithiasis. Comptes Rendus Chimie. 2016;19:1470–91.
– Curhan GC, Willett WC, Knight EL, Stampfer MJ. Dietary factors and the risk of incident kidney stones in younger women. Arch Intern Med. 2004;164:885‑891.
– Khan SR, Canales BK, Domínguez‑Gutiérrez PR. Randall’s plaque and calcium oxalate stone formation: role for immunity and inflammation. Nat Rev Nephrol. 2021;17:417‑433.
– Douketis JD, Spyropoulos AC, Kaatz S, et al. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373:823–833.
– Pauchard F, Ventimiglia E, Corrales M, Traxer O. A Practical Guide for Intra‑Renal Temperature and Pressure Management during RIRS: What Is the Evidence Telling Us. J Clin Med. 2022;11:3429.
– Zhu W, Liu S, Cao J, et al. Tip bendable suction ureteral access sheath versus traditional sheath in retrograde intrarenal stone surgery: an international multicentre, randomized, parallel group, superiority study. EClinicalMedicine. 2024;74:102724.
(For a full reference list, see the ESD 2025 publication cited above.)
Conclusions
ESD 2025 provides a clinician‑focused synthesis of current evidence and expert opinion for the diagnosis, prevention and interventional management of urinary stones. Its key messages are straightforward: (1) evaluate every patient with stone analysis and appropriate metabolic testing; (2) personalize prevention (hydration, diet, citrate and other agents where indicated); (3) adopt device innovations (suction sheaths, DISS, ultra‑slim fURS) thoughtfully to improve stone free rates while minimizing pressure/thermal injury; and (4) balance efficacy, safety and cost. The ESD panel emphasizes pragmatic implementation: use morpho‑compositional data to guide therapy, monitor intrarenal pressure and temperature during endoscopic procedures, and prioritize patient adherence through education and digital tools. Future research priorities include large randomized comparisons of suction‑enabled RIRS vs PCNL for medium‑sized stones, safety studies on laser thermal effects in humans, and randomized trials of phytate and theobromine for prevention.
Practical resources
Clinicians should consult the full EAU 2025 guideline and the ESD 2025 publication for protocol templates, recommended metabolic panels, and device‑specific technical considerations. Multidisciplinary coordination (urology, nephrology, infectious disease, radiology and anesthesia) remains central to safe, effective care.
Reference
Papatsoris A, Geavlete B, Radavoi GD, Alameedee M, Almusafer M, Ather MH, Budia A, Cumpanas AA, Kiremi MC, Dellis A, Elhowairis M, Galán-Llopis JA, Geavlete P, Guimerà Garcia J, Isern B, Jinga V, Lopez JM, Mainez JA, Mitsogiannis I, Mora Christian J, Moussa M, Multescu R, Oguz Acar Y, Petkova K, Piñero A, Popov E, Ramos Cebrian M, Rascu S, Siener R, Sountoulides P, Stamatelou K, Syed J, Trinchieri A. Management of urinary stones by experts in stone disease (ESD 2025). Arch Ital Urol Androl. 2025 Jun 30;97(2):14085. doi: 10.4081/aiua.2025.14085. Epub 2025 Jun 30. PMID: 40583613.