Highlight
- High-dose inactivated influenza vaccine (HD-IIV) significantly reduces hospitalizations related to influenza and cardiovascular (CV) events compared to standard-dose vaccine (SD-IIV) in adults aged 65 and older.
- This large pragmatic randomized trial included over 10,000 participants with heart failure (HF) and demonstrated similar protective effects of HD-IIV across HF subgroups, regardless of disease severity or treatment.
- Findings support HD-IIV as a superior preventive strategy to reduce influenza-triggered CV complications and HF hospitalizations in a high-risk population.
Study Background and Disease Burden
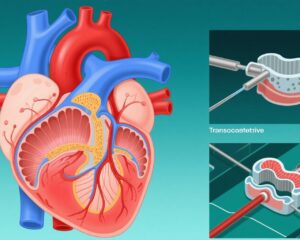
Influenza infection remains a considerable public health challenge globally, with significant morbidity and mortality, particularly among older adults and those with chronic cardiovascular diseases such as heart failure (HF). Influenza triggers systemic inflammation, hemodynamic stress, and myocardial injury, which can precipitate acute decompensations of HF and increase risk for cardiovascular (CV) events including myocardial infarction, stroke, and worsening heart failure hospitalizations. Despite existing guideline recommendations advocating for annual influenza vaccination using standard-dose inactivated vaccines (SD-IIV) in individuals with HF, immune responses to vaccination in this population may be suboptimal due to immunosenescence and HF-related immune dysregulation.
High-dose inactivated influenza vaccine (HD-IIV), containing four times the antigen content of SD-IIV, has been developed to enhance immunogenicity and clinical effectiveness in older adults but its impact specifically in HF patients had not been conclusively established. The DANFLU-2 trial addresses this gap by evaluating whether HD-IIV reduces influenza-related and CV hospitalizations compared to SD-IIV in an elderly Danish population, with a focus on those with baseline HF.
Study Design
The DANFLU-2 trial was a large-scale, pragmatic, prospective, individually randomized, open-label study conducted across Denmark during three consecutive influenza seasons from 2022/2023 through 2024/2025. The trial enrolled community-dwelling citizens aged 65 years and older, randomizing them 1:1 to receive either HD-IIV or SD-IIV.
Endpoints were robustly ascertained by linkage to Danish national healthcare registries, allowing comprehensive detection of hospitalizations related to influenza illness, laboratory-confirmed influenza (LCI), any cardiovascular disease, cardio-respiratory disease, and HF-specific hospitalizations. The study also examined effect modification by HF status at baseline and stratified analyses by HF duration, recent hospitalization, biomarker levels (N-terminal pro-B-type natriuretic peptide), and device therapies.
This prespecified sub-analysis focused on 10,410 participants with diagnosed HF at baseline (27.4% female, mean age 76.0 ± 6.3 years), comparing clinical outcomes against those without HF.
Key Findings
The trial enrolled a total of 332,438 participants (48.6% female, mean age 73.7 ± 5.8 years), including the HF subgroup. Across the entire cohort, HD-IIV recipients demonstrated statistically significant reductions in hospitalization incidence for influenza-related illness, LCI, cardio-respiratory disease, CV disease, and HF events compared to SD-IIV recipients.
Among participants with HF, risk ratios (RR) for HD-IIV versus SD-IIV were consistent and pointed toward meaningful clinical benefit though some confidence intervals included the null value, reflecting limited power in this subgroup:
- Influenza-related hospitalization: RR 0.48 (95% CI, 0.20–1.06; pinteraction=0.64)
- LCI hospitalization: RR 0.55 (95% CI, 0.29–1.02; pinteraction=0.59)
- Cardio-respiratory hospitalization: RR 0.89 (95% CI, 0.77–1.02; pinteraction=0.34)
- CV hospitalization: RR 0.86 (95% CI, 0.72–1.02; pinteraction=0.34)
- HF hospitalization: RR 0.82 (95% CI, 0.61–1.11; pinteraction=0.83)
No statistically significant interactions by HF status were observed, suggesting similar vaccine effectiveness among those with and without HF.
Subgroup analyses stratified by heart failure characteristics including disease duration (recent versus remote diagnosis), recent HF hospitalization, the most recent N-terminal pro-B-type natriuretic peptide levels, and presence of cardiac device therapy revealed consistent point estimates favoring HD-IIV without notable heterogeneity.
Safety data were not highlighted in this analysis but previous studies confirm an acceptable safety profile of HD-IIV in older adults.
Expert Commentary
This prespecified exploratory analysis from the DANFLU-2 trial constitutes the largest randomized evaluation of influenza vaccine dosing strategies in adults with HF to date. The findings align with prior evidence that high-dose influenza vaccines elicit stronger immune responses and higher seroprotection rates in elderly populations, including those with chronic cardiovascular conditions. Given the increased vulnerability of HF patients to influenza-triggered decompensations and cardiovascular events, enhanced immunogenicity conferred by HD-IIV likely translates into meaningful clinical advantages.
While confidence intervals in some HF subgroup analyses crossed unity, the consistent direction and magnitude of effect coupled with no significant interaction by HF status bolster the robustness of the findings. The pragmatic design and registry-based outcome ascertainment ensure strong external validity to routine clinical practice. However, the open-label approach may introduce some bias, though hospitalizations and laboratory confirmations are objective outcomes.
These results support reconsideration of vaccine strategies in HF patients and potentially broaden recommendations for HD-IIV use to this high-risk group. Mechanistically, influenza-induced systemic inflammation and endothelial dysfunction may precipitate HF exacerbations and acute CV events, which can be mitigated by more effective vaccine-induced immunity.
Conclusion
The DANFLU-2 trial prespecified analysis demonstrates that high-dose influenza vaccination offers superior protection against influenza-related illness and cardiovascular complications compared to standard-dose vaccination in adults 65 years and older, including those with heart failure. The similar effectiveness across HF subgroups reinforces the generalizability of this preventive strategy.
Given the substantial burden of influenza-triggered adverse cardiovascular outcomes in HF populations, these findings advocate for integrating high-dose influenza vaccination into routine care paradigms to reduce hospitalizations and improve health outcomes. Further studies exploring cost-effectiveness and long-term benefits could support policy adjustments and guideline updates.
References
Skaarup KG, Johansen ND, Modin D, et al. High-Dose vs. Standard-Dose Influenza Vaccine in Heart Failure: A Prespecified Analysis of the DANFLU-2 Trial. Circ Heart Fail. 2025 Aug 30. doi: 10.1161/CIRCHEARTFAILURE.125.013678. Epub ahead of print. PMID: 40884411.
Chung JR, Flannery B, Belongia EA, et al. Effectiveness of Influenza Vaccine in Preventing Hospitalization Among Adults With Cardiovascular Disease: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2019;8(9):e012560.
Clarisse M, Esposito-Farese MC, Jacques D, et al. Immunogenicity and Safety of High-Dose Influenza Vaccine in Cardiovascular Patients: A Systematic Review. Vaccine. 2021;39(28):3777-3785.
Thompson WW, Shay DK, Weintraub E, et al. Mortality Associated With Influenza and Respiratory Syncytial Virus in the United States. JAMA. 2003;289(2):179-186.
Monto AS, Ohmit SE, Petrie JG, et al. Comparative Efficacy of Inactivated and Live Attenuated Influenza Vaccines. N Engl J Med. 2009;361(13):1260-1267.
Grohskopf LA, Alyanak E, Broder KR, et al. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices—United States, 2023–24 Influenza Season. MMWR Recomm Rep 2023;72(No. RR-3):1–33.