Study Background and Disease Burden
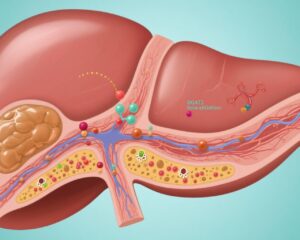
Metabolic dysfunction-associated steatohepatitis (MASH) is an advanced form of nonalcoholic fatty liver disease (NAFLD), characterized by hepatic inflammation, ballooning degeneration, and fibrosis. It is closely associated with metabolic syndrome components such as obesity, type 2 diabetes, and dyslipidemia. MASH leads to progressive liver damage and is a leading cause of liver-related morbidity and mortality, including cirrhosis and hepatocellular carcinoma. Currently, few effective pharmacologic treatments are approved, particularly ones that demonstrably reverse fibrosis, a key predictor of adverse outcomes. This underscores an urgent unmet need for effective, well-tolerated therapies that target the pathological pathways underlying MASH and fibrosis progression.
Efruxifermin is a novel bivalent fibroblast growth factor 21 (FGF21) analogue designed to improve metabolic homeostasis and reduce liver injury. FGF21 analogues have shown potential to modulate lipid and glucose metabolism, reduce hepatic steatosis, and attenuate fibrosis, making efruxifermin a promising candidate for MASH treatment. The HARMONY trial was conducted to prospectively evaluate the long-term safety and efficacy of once-weekly subcutaneous efruxifermin in adults with biopsy-confirmed MASH complicated by moderate to severe fibrosis (stage F2 or F3).
Study Design
HARMONY was a multicentre, randomized, double-blind, placebo-controlled, phase 2b clinical trial carried out across 41 academic and community centers in the USA. Eligible participants were adults aged 18 to 75 years with a liver biopsy confirming MASH, defined by a NAFLD activity score ≥4, with at least score 1 for steatosis, ballooning, and lobular inflammation, and fibrosis staging of F2 or F3 according to histological assessment.
Participants (n=128) were randomized in a 1:1:1 ratio to receive 28 mg efruxifermin, 50 mg efruxifermin, or placebo via subcutaneous injection once weekly. The randomization process was conducted through an interactive response system, ensuring allocation concealment. Blinding was maintained for participants, clinical investigators, site personnel, pathologists performing biopsy assessments, and the sponsor, thereby minimizing bias.
The primary endpoint, previously reported at 24 weeks, was a histological improvement defined as at least one-stage reduction in liver fibrosis without worsening of MASH. For this 96-week extended analysis, key endpoints included the final evaluation of the primary outcome after prolonged treatment, as well as the proportion achieving MASH resolution without fibrosis worsening. Safety assessments comprised adverse event monitoring focused on drug-related effects, particularly liver safety and gastrointestinal tolerability.
Key Findings
Between March 22, 2021, and February 7, 2022, 128 participants were enrolled and randomized; 126 received at least one dose of study medication and were included in the modified intention-to-treat (mITT) population. Among these, 62% were female and 38% male.
At week 96, analysis of the mITT population showed that fibrosis improvement (≥1-stage decrease) without MASH worsening occurred in 8 of 43 participants (19%) in the placebo group, 12 of 40 (30%) receiving 28 mg efruxifermin (a non-significant 12 percentage point increase compared with placebo; 95% CI -6 to 31; p=0.19), and 21 of 43 (49%) receiving 50 mg efruxifermin (a statistically significant 31 percentage point increase versus placebo; 95% CI 12 to 49; p=0.0030).
When restricting analysis to 88 participants with available week-96 biopsies, rates of fibrosis improvement without MASH worsening were 24% (8 of 34) for placebo, 46% (12 of 26) for 28 mg (borderline significance; difference 22 percentage points, 95% CI -1 to 45; p=0.070), and 75% (21 of 28) for 50 mg (highly significant difference of 52 percentage points, 95% CI 31 to 73; p<0.0001).
Regarding safety, adverse events were reported in 95% of participants receiving 28 mg, 100% receiving 50 mg, and 98% in the placebo group. The majority were mild to moderate gastrointestinal events, which were more frequent in the efruxifermin groups compared to placebo. Importantly, there were no cases of drug-induced liver injury or deaths observed throughout the study period, suggesting a favorable safety profile.
Additional secondary outcomes such as biochemical markers of liver function and metabolic parameters were not detailed in the reported results but warrant further exploration.
Expert Commentary
The HARMONY trial’s 96-week data add robust evidence supporting the potential of efruxifermin as a disease-modifying agent in MASH. The observed dose-dependent improvement in fibrosis without worsening of MASH activity suggests a meaningful clinical benefit, especially at the 50 mg weekly dose. These findings align with the hypothesized mechanisms of FGF21 analogues in modulating metabolic and fibrotic pathways.
Notably, the relatively high rate of adverse events with efruxifermin is consistent with class effects, predominantly gastrointestinal symptoms, which appear manageable and do not detract from the overall safety signal. The absence of hepatotoxicity is reassuring, given the liver-centered pathology in MASH.
However, cautious interpretation is warranted due to some limitations: the relatively small sample size especially in subgroup biopsy analyses, the potential for selection bias as not all participants completed biopsies at week 96, and the lack of detailed secondary endpoint data in the report. The modest fibrosis improvement rate in the 28 mg group and borderline statistical results indicate a possible dose threshold for efficacy.
Future phase 3 trials should validate these findings in larger, more diverse cohorts and incorporate comprehensive assessments of metabolic effects, patient-reported outcomes, and long-term safety.
Conclusion
The HARMONY phase 2b trial confirms that once-weekly subcutaneous efruxifermin, particularly at 50 mg dose, significantly improves liver fibrosis in adults with MASH complicated by moderate-to-severe fibrosis over a 96-week treatment period, without worsening steatohepatitis and with an acceptable safety profile. These promising results justify advancing efruxifermin into phase 3 studies, representing an important step toward addressing the substantial unmet need for effective MASH therapeutics focused on fibrosis regression.
References
1. Noureddin M, Frias JP, Neff GW, et al. Safety and efficacy of once-weekly efruxifermin versus placebo in metabolic dysfunction-associated steatohepatitis (HARMONY): 96-week results from a multicentre, randomised, double-blind, placebo-controlled, phase 2b trial. Lancet. 2025 Aug 16;406(10504):719-730. doi:10.1016/S0140-6736(25)01073-6. PubMed PMID: 40818852.
2. Younossi ZM, et al. Nonalcoholic steatohepatitis: clinical assessment and management. Hepatology. 2018;67(1):92-102.
3. Friedman SL, et al. Mechanisms of NAFLD development and therapeutic strategies. Nat Med. 2018;24(7):908-922.
4. Kim S, et al. Fibroblast growth factor 21 as a therapeutic target for metabolic diseases. Curr Opin Investig Drugs. 2014;15(10):945-953.