Highlight
- Verum acupuncture significantly reduced postconcussion syndrome (PCS) symptoms compared to sham and waiting-list controls in mild traumatic brain injury (mTBI) patients.
- Improvements in fractional anisotropy (FA) of key white matter regions, especially the right posterior corona radiata, were observed on MRI following acupuncture therapy.
- These neuroimaging improvements correlated strongly with lasting clinical symptom improvement at 6-12 month follow-up.
- Acupuncture offers a minimally invasive, well-tolerated intervention with potential to enhance long-term neurological recovery after mTBI.
Study Background and Disease Burden
Mild traumatic brain injury (mTBI) constitutes approximately 80%-90% of all traumatic brain injuries worldwide, presenting a major public health challenge. Despite its frequency, mTBI often results in heterogeneous and persistent postconcussion syndrome (PCS), characterized by headaches, cognitive deficits, fatigue, dizziness, and emotional disturbances. The complex and variable nature of PCS has limited the effectiveness of conventional treatment options, which primarily focus on symptomatic management without targeting underlying neuropathology.
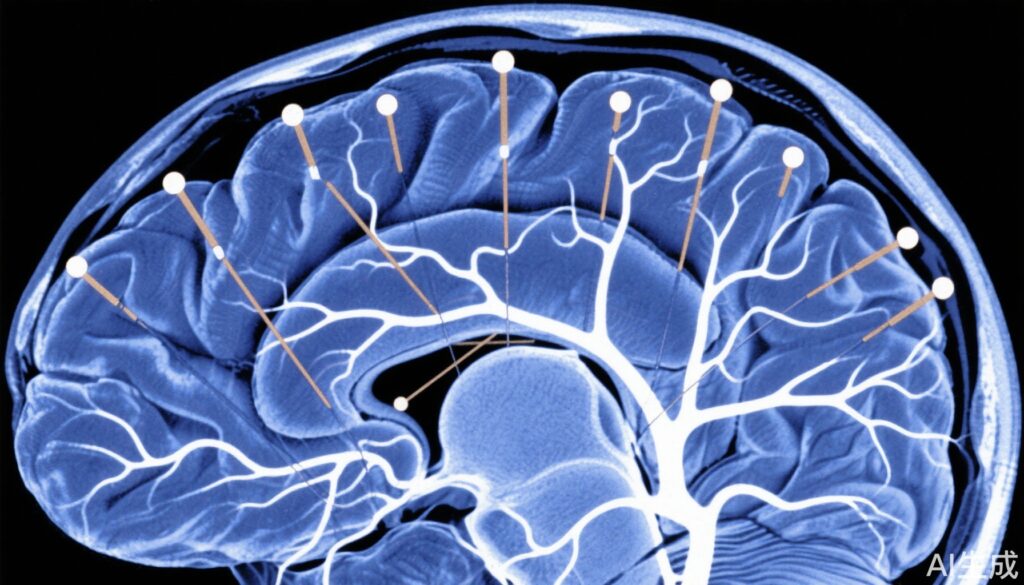
Advanced magnetic resonance imaging (MRI) techniques have revealed microstructural white matter abnormalities in mTBI patients correlating with PCS severity. Fractional anisotropy (FA), derived from diffusion tensor imaging (DTI), serves as an index of white matter integrity, typically reduced in mTBI-related brain injury.
Acupuncture, a traditional Chinese medical intervention, has gained interest as a complementary therapy for neurological disorders. It is minimally invasive, has a favorable safety profile, and may modulate central nervous system function. However, robust clinical evidence supporting its efficacy in mTBI and demonstrating underlying neurobiological mechanisms remains limited.
Study Design
This prospective, randomized, controlled trial enrolled 66 participants with mTBI diagnosed from August 2016 to September 2020. Participants were randomized into three groups: verum acupuncture (n=22), sham acupuncture (n=22), and waiting-list control (n=22). A healthy control group was included for imaging comparisons.
The acupuncture intervention consisted of 14 sessions delivered over 4 weeks. PCS symptoms were evaluated using standardized assessments at baseline, immediately post-therapy, and at 6 to 12 months follow-up. MRI scans were obtained at baseline and post-therapy, focusing on diffusion tensor imaging metrics to assess brain microstructure changes.
Repeated-measures analysis of variance (ANOVA) evaluated changes in PCS scores and MRI metrics across groups and over time. Correlations between imaging changes and clinical outcomes were also analyzed.
Key Findings
The study population had a mean age of 41.2 years (±12.7), balanced by gender (48% male, 52% female). Baseline PCS scores were comparable across intervention arms.
Post-intervention, the verum acupuncture group demonstrated a significant reduction in PCS scores (-5.2 ± 6.9; P=0.002), whereas sham acupuncture (-1.2 ± 6.4) and waiting-list controls (-1.5 ± 5.0) did not achieve significant symptom change (both P > 0.05).
Notably, at 6 to 12 months follow-up, only the verum acupuncture group showed sustained improvement with further PCS score reduction (-8.1 ± 8.6; P<0.001). Sham and waiting-list groups showed no sustained benefit.
MRI analyses revealed that all mTBI participants, compared to healthy controls, exhibited decreased fractional anisotropy in the right cerebral peduncle, anterior limb of the internal capsule, posterior corona radiata (PCR), and cingulum-hippocampus—white matter regions implicated in neurocognitive function.
Crucially, in the verum acupuncture group, significant increases in FA, particularly in the right posterior corona radiata, correlated strongly with long-term symptom improvement (r=0.723; P<0.001). This suggests that acupuncture contributes to white matter microstructural recovery associated with clinical benefit.
Safety data showed that acupuncture was well tolerated without serious adverse events.
Expert Commentary
This rigorous randomized controlled trial provides compelling evidence linking acupuncture to improved neuroimaging biomarkers and clinical outcomes in mTBI—areas where treatment options have been limited. The observed white matter changes support mechanistic plausibility that acupuncture modulates neuroplasticity and may facilitate remyelination or axonal repair processes.
While sham acupuncture controlled for nonspecific effects, this study highlights true physiological benefits distinct from placebo. The durability of effects at 6-12 months emphasizes acupuncture’s potential role in long-term recovery strategies.
Limitations include a relatively small sample size and single-center design, warranting multi-center validation. The heterogeneity of PCS and individual neuroanatomy emphasizes need for future studies to investigate personalized acupuncture protocols.
The findings align with emerging literature on neuroinflammation modulation and autonomic regulation by acupuncture, reinforcing integrative approaches in mTBI care.
Conclusion
This study demonstrates that acupuncture not only reduces the clinical burden of postconcussion symptoms in patients with mild traumatic brain injury but also enhances brain white matter microstructural integrity as measured by MRI. These improvements are sustained longitudinally and correlate with meaningful symptom relief, supporting acupuncture as a promising adjunct therapy for mTBI.
The integration of acupuncture into rehabilitation paradigms could address unmet needs in neurotrauma care, mitigate long-term disability, and improve quality of life. Future larger-scale trials and mechanistic research are needed to optimize protocols and elucidate underlying biological pathways.
References
Wang ZN, Ding JR, Li X, Shi L, Yin B, Bai GH, Fang M, Lao LX, Tian J, Bai LJ. Acupuncture Improves MRI Brain Microstructure with Postconcussion Symptoms in Mild TBI: A Randomized Controlled Trial. Radiology. 2025 Jul;316(1):e250315. doi: 10.1148/radiol.250315. PMID: 40693935.