Study Background and Disease Burden
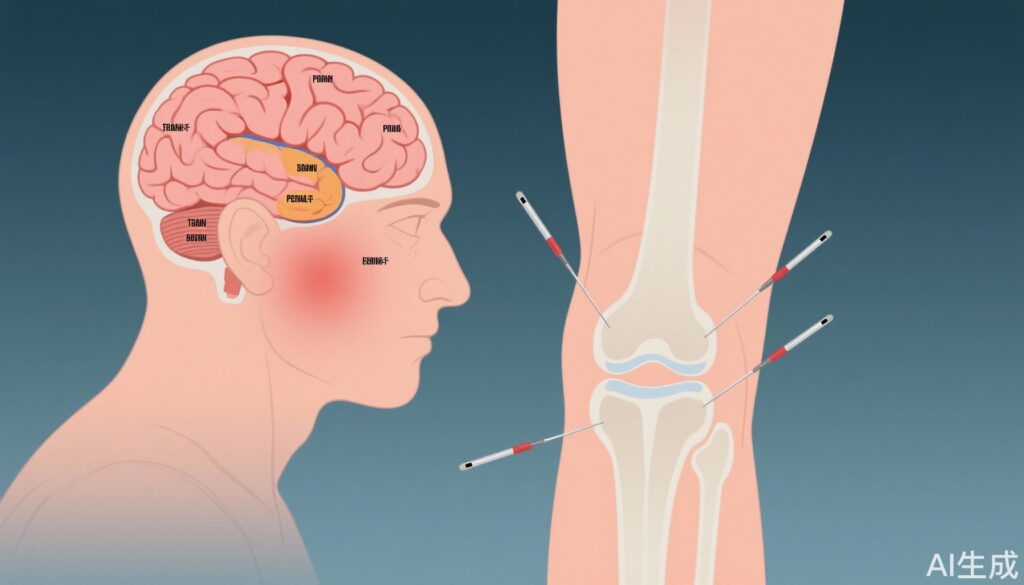
Knee osteoarthritis (KOA) is a prevalent degenerative joint disorder causing chronic pain, reduced mobility, and significant dysfunction, affecting millions worldwide and imposing substantial socioeconomic burdens. Current treatment options, including pharmacotherapy and physical therapy, often provide limited relief or are accompanied by adverse effects. Emerging non-pharmacological interventions such as transcranial direct current stimulation (tDCS), a neuromodulation technique applying low-intensity electrical currents to modulate cortical excitability, and acupuncture, an ancient traditional therapy targeting peripheral and central pain pathways, have shown promise individually in alleviating KOA symptoms. However, their combined effects on clinical outcomes and underlying brain network functional connectivity remain insufficiently explored.
Study Design
This single-center, randomized controlled trial was conducted at the Affiliated Hospital of North Sichuan Medical College between May 2023 and August 2024. Sixty-three patients diagnosed with knee osteoarthritis were recruited from the Departments of Rehabilitation, Orthopedics, and Pain Management. Participants were randomly allocated into three groups: acupuncture only, tDCS only, and combined therapy (acupuncture plus tDCS). Interventions were delivered five times weekly for two consecutive weeks. Clinical assessments included the visual analog scale (VAS) for pain, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) for joint function, and the Lequesne index for disability evaluation. Functional near-infrared spectroscopy (fNIRS) assessed cerebral functional connectivity before and after treatment, focusing on oxyhemoglobin (HbO2) and deoxyhemoglobin (HbR) signals across key brain regions implicated in pain processing and motor control: the left and right prefrontal cortices (LPFC and RPFC) and motor cortices (LMC and RMC).
Key Findings
Out of 63 recruited patients, 60 completed the full treatment and follow-up protocol, with three exclusions due to non-medical reasons such as work commitments and procedural anxiety. All treatment groups showed statistically significant reductions in VAS, WOMAC, and Lequesne scores post-intervention (P < 0.01), indicating effective symptom relief and improved joint function.
Crucially, the combined therapy group exhibited superior improvements compared with either monotherapy group. Specifically, reductions in pain intensity (VAS), functional impairment (WOMAC), and overall disability (Lequesne index) were significantly greater (P < 0.05) in the combined group.
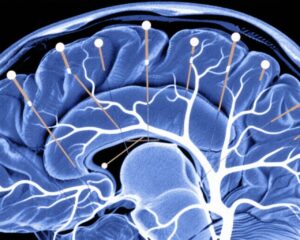
Functional connectivity analyses via fNIRS revealed a significant decrease in mean cerebral connectivity strength across all groups (P < 0.05), suggesting modulation of brain network activity related to KOA symptoms. Compared to acupuncture alone, the combined group demonstrated markedly lower HbO2- and HbR-based functional connectivity within and between bilateral prefrontal and motor cortices (LPFC, RPFC, LMC, RMC), encompassing intra- and inter-hemispheric pathways (P < 0.05). Compared to tDCS alone, the combined group also showed significantly reduced HbO2-based intra-regional connectivity, particularly within prefrontal and motor areas (P < 0.01), reflecting a more robust modulation of cortical networks.
Moreover, the tDCS monotherapy group exhibited lower HbR-based functional connectivity in selected areas (LPFC and LMC) compared to acupuncture (P < 0.05), indicating its distinct neuromodulatory profile.
These data collectively suggest that combined tDCS and acupuncture therapy yields enhanced clinical benefit in KOA by synergistically attenuating aberrant cerebral functional connectivity linked with pain and motor dysfunction.
Expert Commentary
The integration of neuromodulatory and traditional acupuncture paradigms represents an innovative approach to managing chronic osteoarthritic pain. The observed association between clinical improvement and decreased functional connectivity in higher-order cortical regions aligns with contemporary theories positing that chronic pain involves maladaptive brain network synchrony. Reducing such hyperconnectivity may underlie symptom amelioration.
However, limitations include the single-center design and short treatment duration, which may impact generalizability and long-term efficacy. Future multicenter trials with extended follow-up and mechanistic exploration using complementary neuroimaging modalities like fMRI could further elucidate the neural substrates of combined intervention benefits.
Conclusion
In patients with knee osteoarthritis, combined transcranial direct current stimulation and acupuncture therapy outperforms either treatment alone in reducing pain and functional impairment. This enhanced efficacy correlates with a pronounced reduction in brain functional connectivity within key cortical networks. These findings support the therapeutic potential of combined neuromodulatory and acupuncture interventions as a novel, non-invasive strategy to improve clinical outcomes in KOA, warranting further validation and optimization in larger clinical settings.
References
Nie Q, He F, Dong L, Lin X, Lin J, Wang Y, Xie Y. Effects of transcranial direct current stimulation combined with acupuncture therapy on brain network functional connectivity in patients with knee osteoarthritis: a single-center randomized controlled trial. J Neuroeng Rehabil. 2025 Jul 14;22(1):160. doi: 10.1186/s12984-025-01692-y. PMID: 40660313; PMCID: PMC12257676.