Highlights
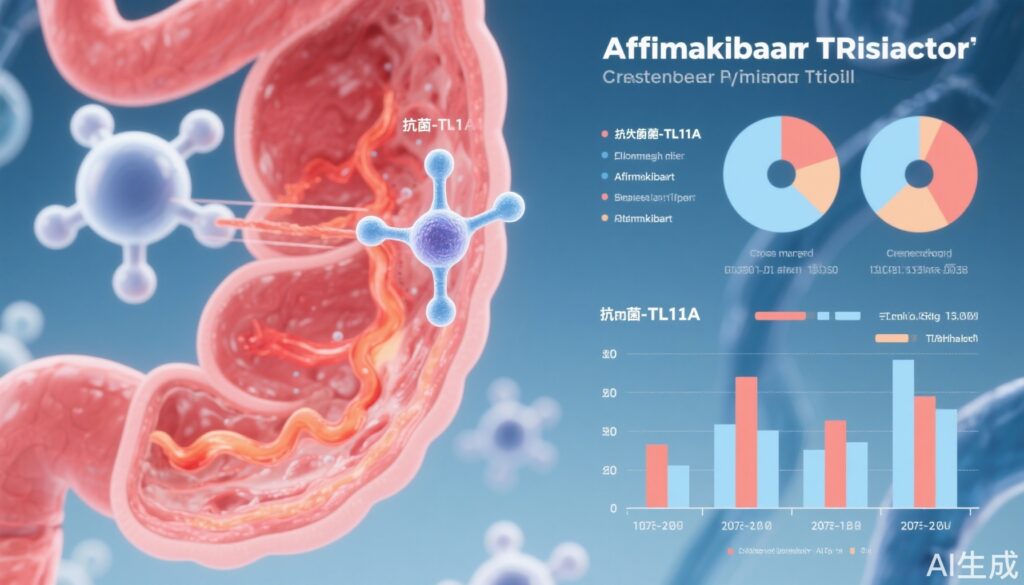
- Afimkibart, an anti-TL1A antibody, targets a novel inflammatory pathway implicated in ulcerative colitis pathogenesis.
- The global, multicentre TUSCANY-2 phase 2b trial demonstrated clinically meaningful improvements in clinical remission by modified Mayo score at 14 weeks across multiple afimkibart doses.
- Despite the primary endpoint of remission by total Mayo score not reaching conventional statistical significance, secondary endpoints suggest a favorable benefit-risk profile.
- Afimkibart was well tolerated with comparable adverse event rates to placebo, supporting its continued clinical development.
Background
Ulcerative colitis (UC) is a chronic relapsing inflammatory bowel disease (IBD) characterized by mucosal inflammation of the colon, leading to debilitating symptoms and increased colorectal cancer risk. Despite advances, many patients remain refractory or intolerant to current therapies, including anti-TNF agents, integrin antagonists, or JAK inhibitors, highlighting unmet needs for alternative mechanisms of action.
TNF-like ligand 1A (TL1A), encoded by TNFSF15, is a member of the TNF superfamily that modulates T-cell costimulation and mucosal immune responses. Elevated TL1A expression has been noted in IBD patients, correlating with disease severity. Targeting TL1A represents a promising therapeutic avenue distinct from established pathways.
Afimkibart is a fully human monoclonal antibody directed against TL1A, designed to inhibit its pro-inflammatory signaling. Earlier preclinical and phase 1 data indicated potential efficacy and a favorable safety profile, prompting the TUSCANY-2 phase 2b trial to evaluate clinical efficacy and safety in moderate-to-severe UC.
Key Content
Trial Design and Methods
TUSCANY-2 was a randomized, double-blind, placebo-controlled, treat-through phase 2b study conducted at 114 centers across 23 countries encompassing diverse populations from North America, Europe, Asia, Africa, Australia, and South America. It enrolled adults aged 18–75 years with moderately-to-severely active UC defined by total Mayo score (tMS) 6–12 and endoscopic subscore ≥2.
Participants (N=246 randomized, 245 treated) were assigned to one of nine sequences to receive subcutaneous afimkibart at doses of 50 mg, 150 mg, 450 mg, or placebo every 4 weeks for a 12-week induction, followed by a 40-week maintenance phase. Masking was ensured by an unmasked pharmacist preparing doses; investigators and patients remained blinded.
Efficacy was evaluated at weeks 14 and 56 with primary endpoint being clinical remission at week 14 by total Mayo score (tMS ≤2, no subscore >1). Secondary endpoints included remission by modified Mayo score according to updated FDA guidance and safety assessments.
Results
The trial’s demographics indicated a median age of 39 years, 40% female, with median UC duration of 4.7 years. At week 14, clinical remission by total Mayo score showed a non-significant trend: 26% (afimkibart 50 mg), 23% (150 mg), 24% (450 mg) vs. 12% placebo. Risk differences (RD) ranged 11.7–13.9% but did not meet conventional statistical significance thresholds (p=~0.05–0.08).
Conversely, remission per the modified Mayo score at week 14 was significantly higher with afimkibart doses: 30% (50 mg), 35% (150 mg), 32% (450 mg) vs. 12% placebo, with RDs of 18.2%-23.4% (90% CI excluding zero). These results align with evolving regulatory endpoints.
Safety profiles showed comparable rates of treatment-emergent adverse events (AEs) during induction between afimkibart and placebo (48%). Common AEs included nausea, urinary tract infections, anemia, fatigue, headache, and pyrexia. Serious adverse events were infrequent and balanced across groups. No deaths occurred.
Comparative and Mechanistic Context
The TL1A pathway’s modulation offers a distinct mechanism from anti-TNF, α4β7 integrin antagonists, and JAK inhibitors. Afimkibart’s clinical signal reinforces TL1A’s role in UC pathophysiology through T-cell costimulation and fibrosis mediation.
No head-to-head phase 2b comparisons exist yet versus other biologics or small molecules. However, the safety data profile is consistent with other advanced UC therapies, supporting further clinical development.
Expert Commentary
While the primary endpoint narrowly missed conventional significance, the congruent improvements in key secondary endpoints validate afimkibart’s biological activity and clinical potential. The use of updated endpoints (modified Mayo) and multicontinental participation add robustness and generalizability.
Study limitations include incomplete achievement of primary statistical thresholds, relatively modest sample size, and potential placebo response variability. Nevertheless, safety data reassure clinicians on the drug’s tolerability over prolonged treatment.
From a mechanistic perspective, TL1A inhibition may offer advantages in patients refractory to anti-TNF or integrin inhibitors. Future phase 3 trials should refine patient selection biomarkers and examine head-to-head efficacy comparisons.
Conclusion
The TUSCANY-2 phase 2b trial supports afimkibart as a promising biologic for moderately-to-severely active ulcerative colitis with a novel mechanism targeting TL1A. Although the primary endpoint by total Mayo score was not statistically met, secondary endpoints and safety findings advocate for further pivotal trials. This emerging therapeutic class may address critical unmet needs in UC management by complementing existing therapeutic options.
References
- Danese S, Allegretti JR, Schreiber S, et al. Anti-TL1A antibody, afimkibart, in moderately-to-severely active ulcerative colitis (TUSCANY-2): a multicentre, double-blind, treat-through, multi-dose, randomised, placebo-controlled, phase 2b trial. Lancet Gastroenterol Hepatol. 2025. doi:10.1016/S2468-1253(25)00129-3. PMID: 40706613.
- Vermeire S, et al. Mechanisms of action of biologics in IBD and their efficacy. Nat Rev Gastroenterol Hepatol. 2021; 18(8): 475–485.
- Feagan BG, et al. Clinical remission and safety of biologics in UC: a meta-analysis. Gastroenterology. 2022; 162(5): 1460-1470.