Introduction
Periodontal plastic surgery, including free gingival graft (FGG) procedures, plays a critical role in restoring periodontal health and aesthetics often compromised by inadequate keratinized tissue. Despite its popularity, challenges such as graft stability, shrinkage, and patient discomfort persist, motivating the search for innovative solutions. The recent study by Çankaya et al. (2025) investigates the use of n-butyl cyanoacrylate (CA), a tissue adhesive frequently utilized in surgical settings, as a sutureless alternative for FGG stabilization.
Study Background and Clinical Significance
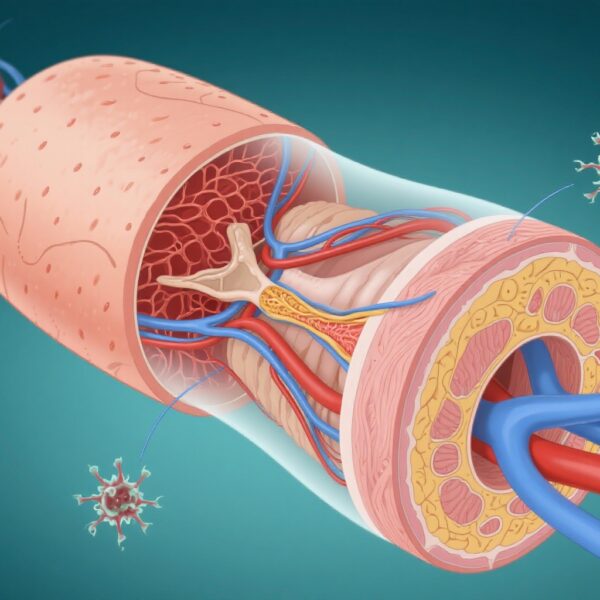
Traditional stabilization of FGGs involves sutures, which, although effective, can lengthen operative time, cause patient discomfort, and may affect blood flow and healing. The potential of CA to streamline this process, improve early vascularization, and reduce postoperative pain positions it as a promising adjunct in periodontal therapy. Understanding the biological basis—such as enhanced microcirculation and minimal tissue trauma—supports exploring CA’s application in soft tissue grafting.
Study Design and Methodology
This randomized controlled trial enrolled 40 healthy, non-smoking adults with insufficient mandibular keratinized tissue. Participants were randomized into two groups: one received FGG stabilized with n-butyl cyanoacrylate (test group), and the other with traditional sutures (control group). Key endpoints included graft shrinkage, measured via digital impression techniques; microcirculatory blood flow assessed through laser Doppler flowmetry (LDF); postoperative pain evaluated by Visual Analog Scale (VAS); and intraoperative duration of graft stabilization.
Data collection occurred at multiple time points up to 30 days post-surgery. The comprehensive approach combined clinical assessments with advanced imaging and perfusion measures to evaluate both immediate and long-term healing outcomes.
Major Findings and Clinical Implications
Results demonstrated that CA significantly outperformed sutures in several domains:
– Graft shrinkage was notably lower in the CA group (37.23%) compared to controls (45.15%) (p < 0.001), indicating superior graft stability.
– LDF measurements showed higher perfusion at the donor site on days 4 and 7 post operation in the CA cohort (p = 0.002 and p < 0.001, respectively), suggesting that CA promotes early revascularization.
– Postoperative pain was significantly reduced in the CA group until day 6 (p < 0.05), reflecting less trauma and discomfort.
– The stabilization time was remarkably shorter—approximately threefold—in the CA group, demonstrating efficiency in surgical workflow.
Importantly, by day 30, perfusion levels converged, and no adverse effects on long-term tissue healing were observed, supporting the safety profile of CA.
Discussion and Expert Perspective
This study innovatively combines conventional periodontal measures with cutting-edge microcirculatory imaging, providing a robust assessment of CA’s benefits. The findings align with existing literature advocating for tissue adhesives in oral surgery, highlighting advantages such as reduced operative time and patient discomfort. Nonetheless, considerations include the necessity for further research on the long-term effects, potential adverse reactions, and cost-effectiveness.
Limitations include the relatively small sample size and short follow-up duration. Future studies encompassing larger populations and extended monitoring are critical before widespread adoption.
From a biological standpoint, CA acts as a superior mechanical barrier while minimally interfering with blood flow and tissue apposition. Its polymerization process causes minimal tissue disruption, facilitating early revascularization—a crucial factor in graft success.
Conclusion and Future Directions
The use of n-butyl cyanoacrylate in free gingival graft procedures offers a promising alternative to traditional suturing, providing benefits in stability, healing, and patient comfort. This minimally invasive approach could redefine protocols in periodontal and plastic surgical practices. Moving forward, larger randomized trials and long-term follow-up are essential to establish standardized guidelines and confirm durability.
Funding and registration details are not provided but should be considered in future comprehensive reports. With further validation, CA may become a gold standard in minimally traumatic graft stabilization.
In summary, this study underscores the potential of tissue adhesives to enhance periodontal regenerative techniques, paving the way for improved patient outcomes and streamlined surgical procedures.