Introduction: The Clinical Conundrum of Post-ICH Atrial Fibrillation
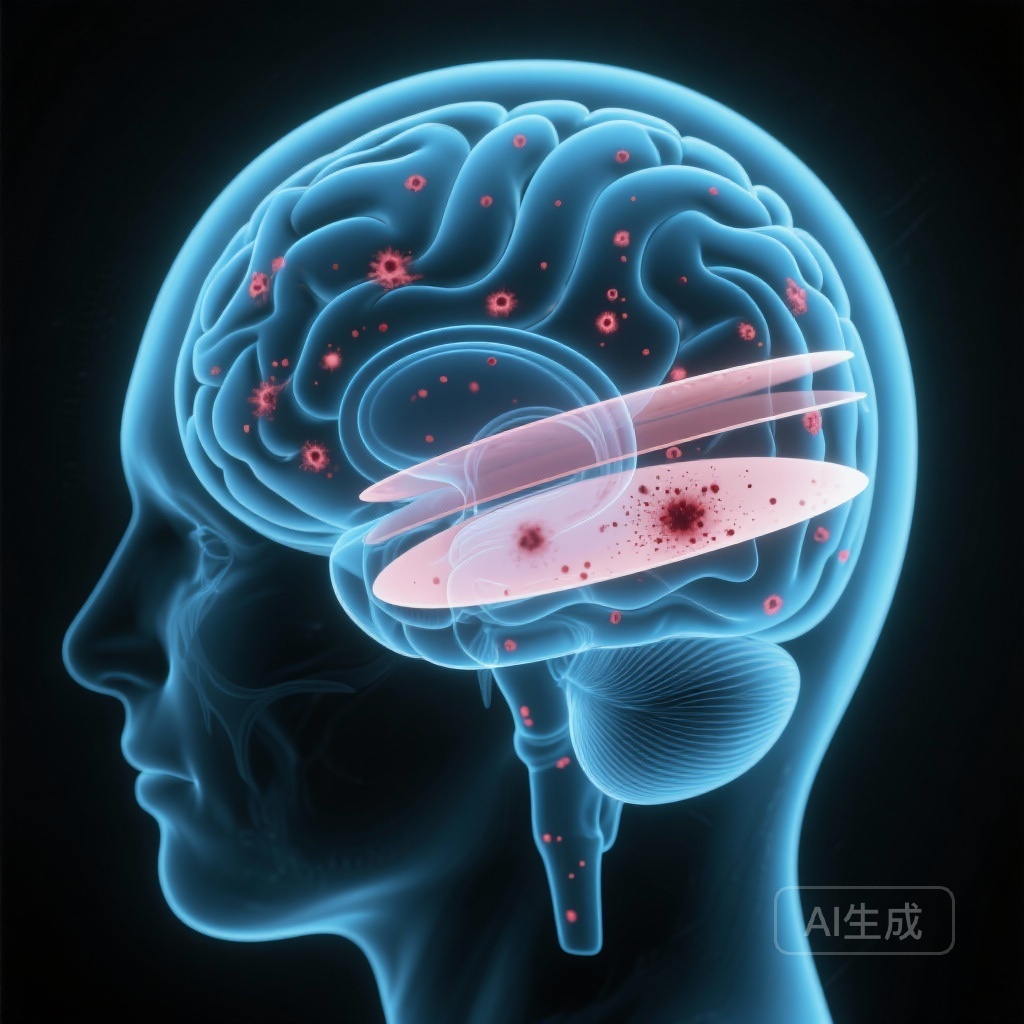
The management of patients with atrial fibrillation (AF) who have survived a spontaneous intracerebral hemorrhage (ICH) represents one of the most challenging dilemmas in contemporary vascular neurology. On one hand, AF significantly elevates the risk of ischemic stroke (IS), necessitating oral anticoagulation (OAC). On the other hand, the history of ICH indicates an underlying cerebral vasculopathy—most commonly hypertensive small vessel disease or cerebral amyloid angiopathy (CAA)—that predisposes the patient to catastrophic bleeding, a risk that may be exacerbated by OAC therapy.
While direct oral anticoagulants (DOACs) have improved the safety profile of anticoagulation compared to vitamin K antagonists, clinical decision-making remains difficult due to the lack of precise risk-stratification tools. Clinicians have traditionally relied on the anatomical location of the primary ICH (lobar vs. nonlobar) to estimate future risks, but this approach is often insufficient. The PRESTIGE-AF trial imaging subanalysis, recently published in Neurology, provides critical insights into how advanced neuroimaging can identify specific markers of susceptibility for both recurrent ICH and ischemic stroke.
Study Highlights
– Cortical superficial siderosis (cSS) and chronic intracerebral macrohemorrhages on MRI are potent predictors of recurrent ICH, with hazard ratios exceeding 7.0.
– Nonlobar ICH location was identified as a significant marker for increased ischemic stroke risk (HR 9.1).
– Traditional anatomical classification (lobar vs. nonlobar) did not significantly predict ICH recurrence in this cohort, suggesting that specific small vessel disease markers are more clinically relevant than the index bleed location.
Study Design and Methodology
PRESTIGE-AF (Prevention of Stroke in Intracerebral Hemorrhage Survivors with Atrial Fibrillation) was a prospective, randomized clinical trial conducted across 75 hospitals in six European countries. The trial randomized participants with a history of spontaneous ICH and a diagnosis of AF to either treatment with DOACs or no anticoagulation.
In this prespecified imaging subanalysis, researchers centrally assessed baseline brain CT and MRI scans from 313 patients (median age 79 years; 35.5% female). MRI was available for 54.3% of the participants. The neuroimaging markers were evaluated using established clinical scales, focusing on markers of cerebral small vessel disease (cSVD), including:
– Hematoma location (lobar vs. nonlobar)
– Cortical superficial siderosis (cSS)
– Cerebral microbleeds (CMBs)
– Chronic intracerebral macrohemorrhages
– Probable cerebral amyloid angiopathy (CAA) status
The primary objective was to investigate the association between these neuroimaging findings and the subsequent occurrence of recurrent ICH and ischemic stroke over a median follow-up period of 1.4 years.
Key Findings: Redefining Risk Stratification
Predictors of Recurrent Intracerebral Hemorrhage
The study found that the simple classification of the index ICH as lobar or nonlobar was not a significant predictor of recurrence (p > 0.2). Similarly, the overall category of ‘probable CAA’ did not reach statistical significance in this cohort for predicting new ICH events. However, specific MRI-defined markers of advanced vasculopathy were highly predictive:
1. Cortical Superficial Siderosis (cSS): Patients with cSS at baseline had a nearly eight-fold increase in the risk of recurrent ICH (Hazard Ratio [HR] 7.7; 95% CI 1.4–42.2).
2. Chronic Macrohemorrhages: The presence of previous large-scale hemorrhages on MRI was even more predictive, associated with a nine-fold risk increase (HR 9.1; 95% CI 1.8–46.8).
These findings suggest that the total burden and specific type of hemorrhagic injury are more indicative of a ‘fragile’ cerebrovascular system than the location of the most recent event.
Predictors of Ischemic Stroke
Interestingly, the imaging markers for ischemic stroke risk differed from those for ICH. The most striking finding was that patients whose index ICH was in a nonlobar (deep) location were at a significantly higher risk for future ischemic stroke (HR 9.1; 95% CI 1.2–67.7). This likely reflects a higher burden of systemic hypertensive vascular disease and atherosclerosis in patients with deep ICH, compared to the more localized amyloid-related pathology often seen in lobar ICH.
Clinical Implications and Mechanistic Insights
The results from PRESTIGE-AF emphasize that MRI is not just a diagnostic tool for the index event but a critical prognostic instrument for long-term management. The high hazard ratios for cSS and macrohemorrhages underscore the importance of identifying these features before initiating or resuming anticoagulation.
The Significance of Cortical Superficial Siderosis
cSS represents blood breakdown products in the subarachnoid space and is a hallmark of advanced CAA. Mechanistically, cSS indicates a chronic leakage from fragile cortical vessels. Its presence suggests a high degree of vascular instability, making the patient particularly vulnerable to the anticoagulant effects of DOACs. The PRESTIGE-AF data suggests that for patients with extensive cSS, the risk-benefit ratio of OAC may shift unfavorably toward bleeding.
The Nonlobar Paradox
The finding that nonlobar ICH predicts ischemic stroke rather than recurrent ICH highlights the systemic nature of hypertensive small vessel disease. These patients may have a higher ‘vascular age’ and more extensive systemic arterial disease, making them prime candidates for aggressive ischemic stroke prevention, provided the risk of recurrent bleeding is managed.
Expert Commentary and Study Limitations
While the findings are compelling, the PRESTIGE-AF consortium acknowledges certain limitations. The most notable is the modest number of outcome events (13 recurrent ICHs and 22 ischemic strokes), which led to wide confidence intervals for the hazard ratios. This limited the ability to perform complex multivariable adjustments and necessitates caution in interpreting the exact magnitude of the risks.
Furthermore, MRI was only available for approximately half of the participants. While this is common in large multicenter trials involving acute ICH, it may introduce selection bias, as patients who are more stable or have fewer contraindications are more likely to undergo MRI.
Clinicians should view these results as a call to move beyond ‘one-size-fits-all’ rules (like the 4-week wait rule or lobar/nonlobar distinctions) and toward a more granular, imaging-based phenotyping of the patient’s brain health.
Conclusion
The PRESTIGE-AF imaging subanalysis demonstrates that neuroimaging markers, particularly those obtained via MRI, are essential for the individualized risk assessment of patients with AF and prior ICH. By identifying cortical superficial siderosis and chronic macrohemorrhages, clinicians can better recognize patients at the highest risk for recurrent ICH. Conversely, the nonlobar location of the index bleed identifies those at particularly high risk for ischemic events. Future large-scale collaborations and pooled analyses will be vital to refining these risk models and establishing definitive guidelines for anticoagulation in this high-stakes patient population.
Funding and Trial Registration
The PRESTIGE-AF trial was funded by the European Union’s Horizon 2020 research and innovation programme. Trial registration: ClinicalTrials.gov NCT03996772.
References
Fandler-Höfler S, Ropele S, Gattringer T, et al. Neuroimaging Markers Associated With Recurrent Stroke in Intracerebral Hemorrhage and Atrial Fibrillation: Secondary Analysis of PRESTIGE-AF. Neurology. 2025 Dec 9;105(11):e214386. doi: 10.1212/WNL.0000000000214386. Epub 2025 Nov 6. PMID: 41197104.