Introduction: The Unmet Need in Richter Transformation
Richter transformation (RT) represents one of the most formidable challenges in modern hematology. Defined as the sudden progression of chronic lymphocytic leukaemia (CLL) or small lymphocytic lymphoma (SLL) into an aggressive lymphoma—most commonly diffuse large B-cell lymphoma (DLBCL)—RT is associated with an exceptionally poor prognosis. Historically, patients with RT have faced a median survival of only 6 to 12 months. This prognosis is further exacerbated in patients who have previously been treated with covalent BTK inhibitors or those harboring high-risk genetic features such as TP53 aberrations or del(17p).
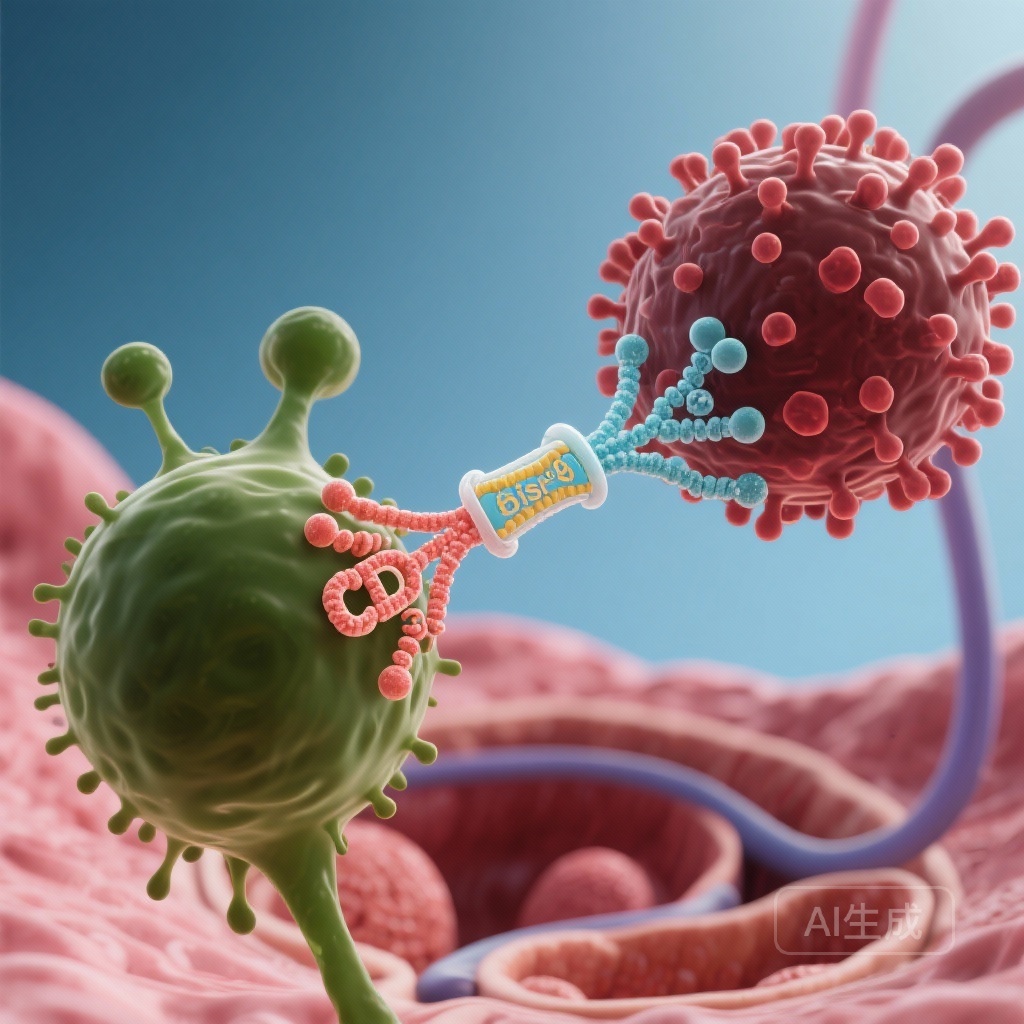
Standard chemoimmunotherapy regimens, such as R-CHOP, often fail to provide durable responses in this population. Consequently, there is an urgent clinical need for novel therapeutic strategies that bypass traditional resistance mechanisms. The EPCORE CLL-1 trial sought to address this by investigating epcoritamab, a first-in-class subcutaneous CD3×CD20 bispecific antibody, as a monotherapy for patients with RT.
Study Design and Patient Population
The EPCORE CLL-1 trial (NCT04623541) is a multicentre, open-label, phase 1b/2 study conducted across 24 centers internationally. The trial was designed with several expansion groups to evaluate epcoritamab both as a monotherapy and in combination with other agents. This report focuses specifically on Group 2A, which evaluated epcoritamab monotherapy.
Patient Eligibility and Baseline Characteristics
Eligible participants were adults with histologically confirmed RT (DLBCL subtype) and an ECOG performance status of 0–2. Notably, the trial permitted patients who had received up to two previous lines of RT-directed therapy.
A total of 42 patients were enrolled between October 2021 and March 2025. The median age was 69 years. The baseline characteristics reflected a high-risk population: the median time from CLL diagnosis to RT was 7.6 years, and 50% of the cohort received epcoritamab as their first-line therapy for RT. Furthermore, 48% of patients (20 out of 42) had TP53 aberrations and/or del(17p) at baseline, a subgroup that typically responds poorly to conventional treatments.
Treatment Protocol
Epcoritamab was administered subcutaneously using a step-up dosing schedule to mitigate the risk of cytokine release syndrome (CRS). Following the step-up phase, patients received a full dose of 48 mg weekly during Cycles 1–3, every two weeks during Cycles 4–9, and every four weeks thereafter until disease progression or intolerable toxicity occurred.
Key Findings: Efficacy and Clinical Response
The primary endpoint of the study was the investigator-assessed overall response rate (ORR) according to Lugano 2014 criteria. The study was powered to test a null hypothesis of a 30% ORR against an alternative hypothesis of 50%.
Overall Response Rates
At a median follow-up of 22.9 months, 20 of the 42 patients achieved a response, resulting in an ORR of 47.6% (95% CI 32.0–63.6). Although this result narrowly missed the prespecified alternative hypothesis of 50%, it represents a clinically significant improvement over historical benchmarks for this refractory population.
Response by Subgroup
Data from prespecified subgroup analyses provided deeper insights into the drug’s activity:
1. First-line RT Therapy: In patients receiving epcoritamab as their first treatment for RT, the ORR was 57.1% (12 of 21 patients).
2. Second-line or Later: For those who had failed previous RT-directed therapies, the ORR was 38.1% (8 of 21 patients).
3. High-Risk Genetics: In the subset of patients with TP53 aberrations and/or del(17p), the ORR remained robust at 40% (8 of 20 patients).
These findings suggest that epcoritamab maintains activity even in the presence of genomic instability that often renders chemotherapy ineffective.
Safety and Tolerability Profile
The safety profile of epcoritamab in the EPCORE CLL-1 trial was consistent with previous reports of bispecific antibodies in other B-cell malignancies.
Adverse Events
The most frequent grade 3–4 adverse events were hematological, including neutropenia (45%), anemia (38%), and thrombocytopenia (38%). Infections were reported in 21% of patients, with pneumonia occurring in 10% and COVID-19 in 5%. Three fatal adverse events occurred during the study (sepsis, cerebrovascular accident, and general health deterioration due to disease progression), but none were attributed to the study treatment by investigators.
Immune-Related Toxicities
Cytokine release syndrome (CRS) occurred in 86% of patients. However, the majority of these events were low-grade; only 7% of patients experienced grade 3 CRS, and no grade 4 or 5 events were reported. The median time to CRS onset was consistent with the step-up dosing schedule, allowing for predictable management.
Immune effector cell-associated neurotoxicity syndrome (ICANS) was observed in 12% of patients (5 out of 42), all of which were grade 1 or 2. Clinical tumour lysis syndrome (TLS) was rare, occurring in only 5% of the cohort (grade 1–2).
Expert Commentary: Interpreting the Data
While the primary endpoint did not strictly meet the 50% alternative hypothesis, the clinical community views these results with cautious optimism. In the context of Richter transformation, where therapeutic options are scarce and outcomes are generally dismal, an ORR of nearly 48% with a monotherapy agent is a notable achievement.
Biological Plausibility
The efficacy of epcoritamab in RT is biologically grounded in its ability to engage host T-cells to target CD20-positive malignant cells directly. Because this mechanism is independent of the DNA-damage response pathways (which are often mutated in RT via TP53 loss), it provides a bypass for chemoresistance. The subcutaneous administration also offers a logistical advantage and potentially a more controlled cytokine release profile compared to intravenous bispecifics.
Study Limitations
The primary limitation of this study is its single-arm design and relatively small sample size (n=42), which is common in rare and aggressive diseases like RT. Additionally, the investigator-assessed ORR might differ slightly from a central independent review, though the clinical signal remains clear.
Conclusion and Future Directions
The EPCORE CLL-1 trial demonstrates that epcoritamab monotherapy provides clinically meaningful antitumor activity in patients with Richter transformation, including those with high-risk genetic features and prior therapy. The manageable safety profile, characterized by predictable CRS and ICANS, supports its potential role in the treatment landscape of this aggressive disease.
Future research is already underway to explore whether combining epcoritamab with other agents—such as lenalidomide (Group 2B) or R-CHOP (Group 2C)—can further improve response rates and durability. For now, epcoritamab stands as a promising addition to the armamentarium against one of hematology’s most difficult-to-treat conditions.
Funding and Trial Registration
This trial was funded by Genmab A/S and AbbVie. ClinicalTrials.gov Identifier: NCT04623541.
References
1. Kater AP, Janssens A, Eradat H, et al. Epcoritamab monotherapy for Richter transformation (EPCORE CLL-1): findings from a single-arm, multicentre, open-label, phase 1b/2 trial. Lancet Haematol. 2026;13(1):e8-e21.
2. Lugano 2014 criteria for response assessment in lymphoma. Journal of Clinical Oncology.
3. Rossi D, et al. The genetics of Richter transformation. Blood. 2018.