The Challenge of Intracranial Atherosclerotic Disease
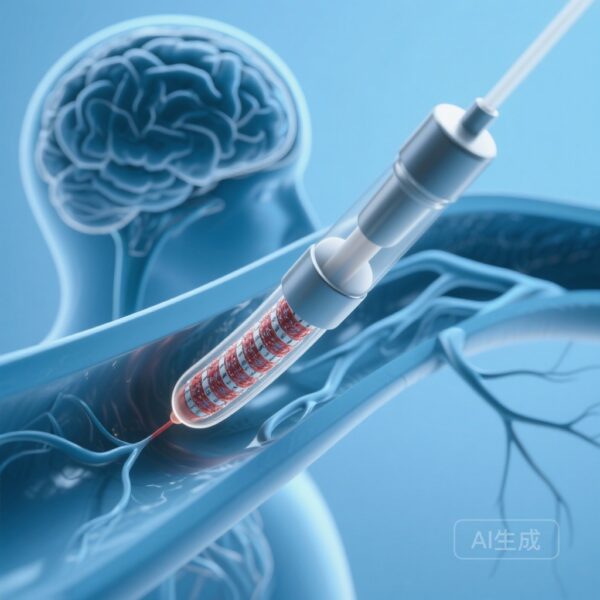
Intracranial atherosclerotic disease (ICAD) remains a formidable challenge in vascular neurology, serving as one of the most common causes of ischemic stroke worldwide. For patients with high-grade symptomatic stenosis, medical management alone often proves insufficient, leading clinicians to explore endovascular interventions. While bare-metal stent (BMS) placement has traditionally provided a mechanical solution to restore luminal diameter, the long-term efficacy of this approach is frequently undermined by in-stent restenosis (ISR). Restenosis, driven by neointimal hyperplasia, is a primary driver of recurrent cerebrovascular events, necessitating more durable therapeutic strategies.
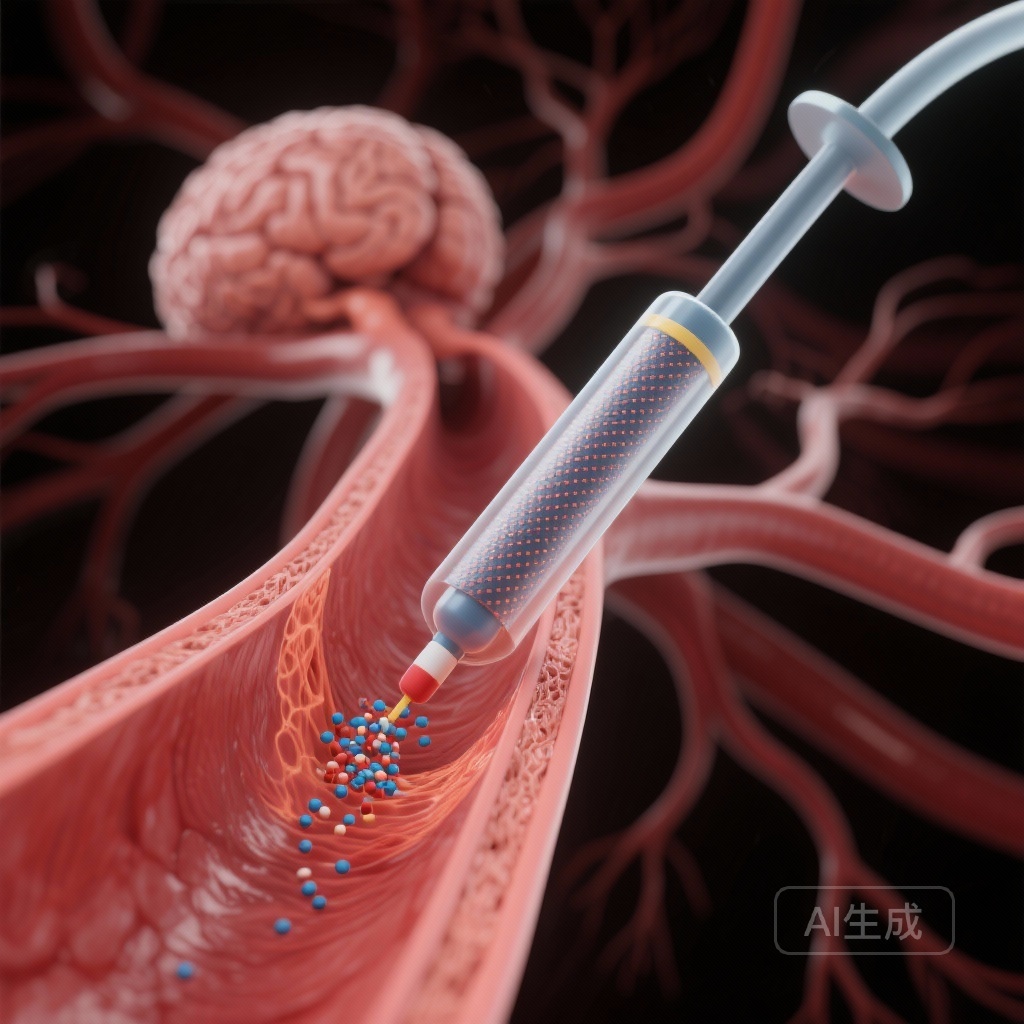
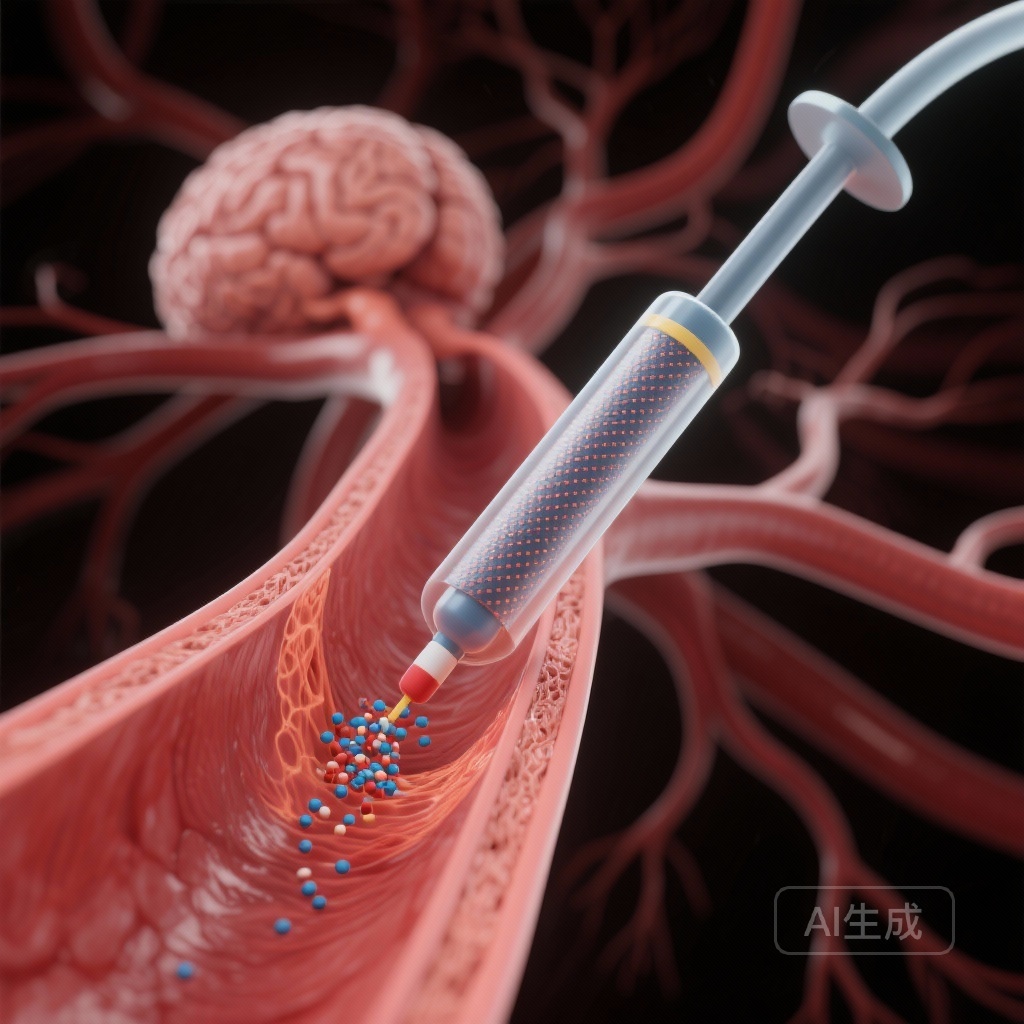
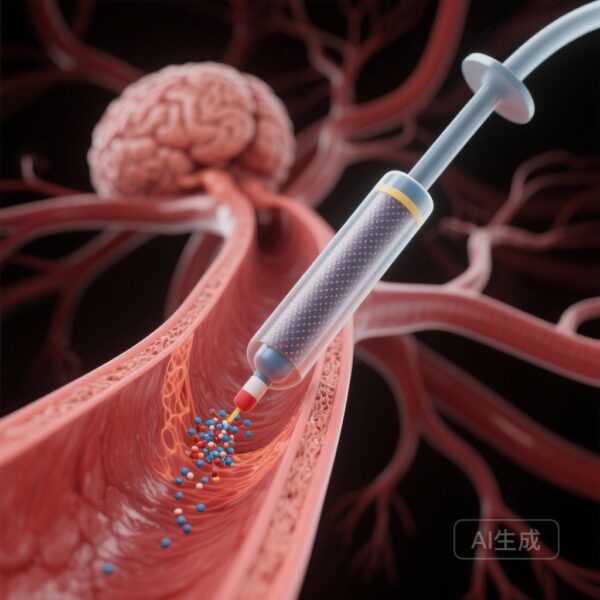
Drug-coated balloons (DCBs), which deliver antiproliferative agents directly to the vessel wall without leaving a permanent metallic scaffold, have revolutionized the treatment of peripheral and coronary artery disease. However, their application in the delicate intracranial circulation has remained a subject of intense investigation. The DR. BEYOND study, a multicenter randomized controlled trial recently published in Radiology, provides landmark evidence comparing DCB angioplasty against traditional BMS placement for symptomatic ICAD.
Study Highlights
The trial yielded several critical insights for the management of high-grade ICAD:
- DCB angioplasty resulted in a significantly lower rate of 6-month angiographic restenosis (11%) compared to BMS placement (29%).
- Symptomatic restenosis at 6 months was markedly reduced in the DCB cohort (1% vs 10%).
- The risk of recurrent ischemic events between 30 days and 1 year was substantially lower for patients treated with DCBs (4% vs 13%).
- Safety outcomes, specifically 30-day stroke or death rates, were comparable between both intervention groups.
Trial Design and Methodology
The DR. BEYOND trial was a prospective, multicenter randomized controlled trial conducted across 14 tertiary hospitals in China. The study enrolled 209 participants between July 2021 and March 2023. Eligible participants were adults with symptomatic ICAD characterized by high-grade stenosis (70%-99%) who had failed medical therapy.
Participants were randomly assigned in a 1:1 ratio to receive either DCB angioplasty (n=103) or BMS placement (n=106). The primary endpoint was the rate of restenosis at 6 months, as determined by digital subtraction angiography (DSA). Secondary endpoints included symptomatic restenosis at 6 months and clinical outcomes such as recurrent ischemic events and mortality up to 1 year. The researchers utilized generalized linear and Cox regression models to evaluate the differences between the two groups, ensuring a robust statistical foundation for the findings.
Efficacy Results: A Significant Clinical Shift
The primary outcome data revealed a clear advantage for DCB angioplasty. Among the 164 participants who completed the 6-month DSA follow-up, the restenosis rate in the DCB group was 11%, whereas the BMS group experienced a 29% restenosis rate. This represents a risk ratio of 0.38 (95% CI: 0.19, 0.78; P = .006), indicating that DCB treatment reduces the risk of restenosis by more than 60% compared to bare-metal stenting.
Clinical efficacy extended beyond imaging findings. Symptomatic restenosis occurred in only 1% of the DCB group compared to 10% in the BMS group (P = .02). Perhaps most importantly for long-term patient care, the rate of recurrent ischemic events from day 30 to one year was significantly lower in the DCB group (4% vs 13%; Hazard Ratio 0.31; P = .04). These findings suggest that the biological action of the drug-coated balloon provides a more stable and lasting therapeutic effect than mechanical stenting alone.
Safety and Procedural Considerations
Safety is a paramount concern in intracranial interventions due to the risk of periprocedural stroke or vessel rupture. The DR. BEYOND trial found that the 30-day stroke or death rate was 6% in the DCB group and 5% in the BMS group. The difference was not statistically significant (Hazard Ratio 1.24; P = .73), suggesting that DCB angioplasty does not introduce additional acute procedural risks compared to the established standard of bare-metal stenting.
The use of DCBs allows for the delivery of paclitaxel, a lipophilic cytotoxic agent that inhibits the migration and proliferation of vascular smooth muscle cells. Unlike a stent, which remains as a foreign body and can trigger a chronic inflammatory response, the DCB leaves nothing behind after the procedure, potentially preserving the natural vasoreactivity of the vessel and reducing the long-term risk of thrombotic complications.
Expert Commentary and Clinical Implications
The results of this trial represent a potential shift in the treatment paradigm for symptomatic ICAD. Historically, the SAMMPRIS and VISSIT trials highlighted the risks of intracranial stenting, leading to a more cautious approach and a preference for aggressive medical management. However, for patients who continue to experience symptoms despite optimal medical therapy, the DR. BEYOND data suggests that DCB angioplasty offers a safer and more effective alternative to bare-metal stents.
Clinicians should note that while the results are promising, the study was conducted in a specific population at high-volume tertiary centers. The generalizability to other ethnic groups or lower-volume centers requires further validation. Additionally, the comparison was made against bare-metal stents; future research comparing DCBs to modern drug-eluting stents (DES) or specialized medical management cohorts would further clarify the optimal role of DCBs in the clinical workflow.
Conclusion
The DR. BEYOND trial provides high-quality evidence that drug-coated balloon angioplasty is superior to bare-metal stent placement for reducing both angiographic and symptomatic restenosis in patients with high-grade symptomatic ICAD. With a significant reduction in 1-year recurrent ischemic events and a safety profile comparable to traditional stenting, DCBs emerge as a highly effective tool in the neuro-interventional armamentarium. As the medical community continues to refine stroke prevention strategies, these findings support the integration of DCB technology into the standard care for refractory intracranial atherosclerotic disease.
Funding and Trial Registration
This study was supported by various national health and research grants in China. The trial is registered with the Chinese Clinical Trial Registry under number ChiCTR2100046829.
References
Guan S, Tong X, Li X, et al. Drug-coated Balloon for Endovascular Treatment of Symptomatic Intracranial Stenotic Disease: A Multicenter Randomized Controlled Trial. Radiology. 2026;318(1):e250893. doi: 10.1148/radiol.250893.