Highlights
- Insulin resistance (measured by HOMA-IR) and insulin secretion (C-peptide) are powerful, independent predictors of impaired heart rate recovery (HRR60) in heart failure patients.
- The association between glycemic status (HbA1c) and cardiac vagal activity appears largely dependent on underlying insulin metabolism.
- C-peptide showed stronger effect estimates than HOMA-IR, highlighting the potential role of endogenous insulin production in autonomic signaling.
- Two-year follow-up data confirm that metabolic dysregulation at baseline predicts persistent or worsening autonomic dysfunction.
Background: The Autonomic-Metabolic Nexus
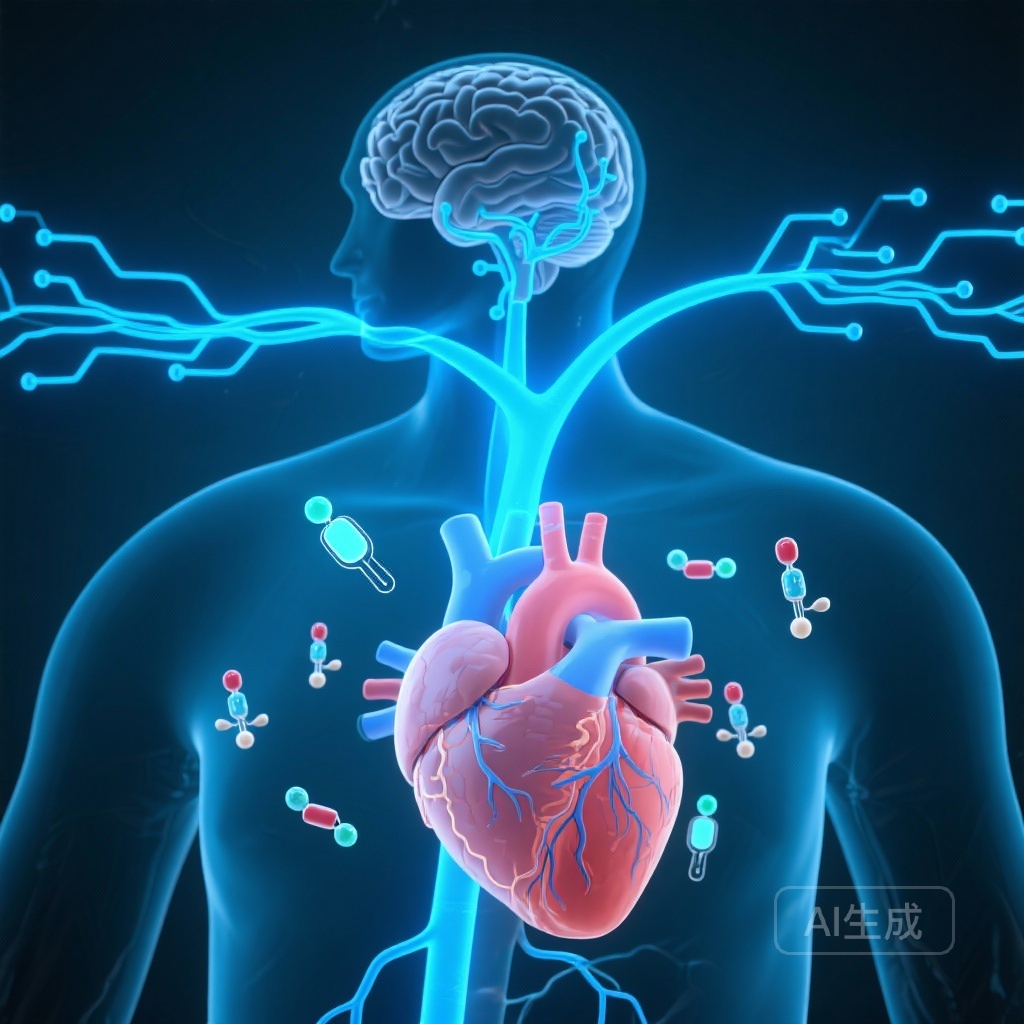
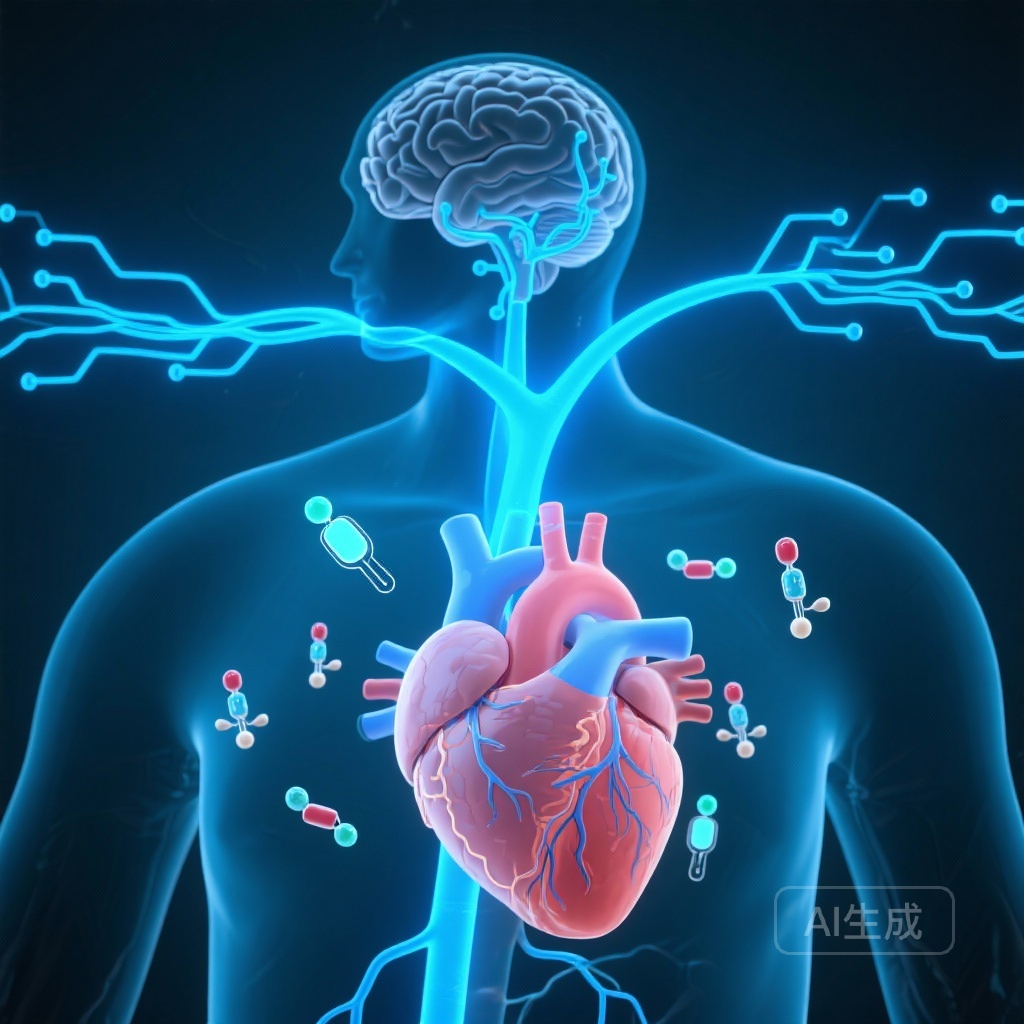
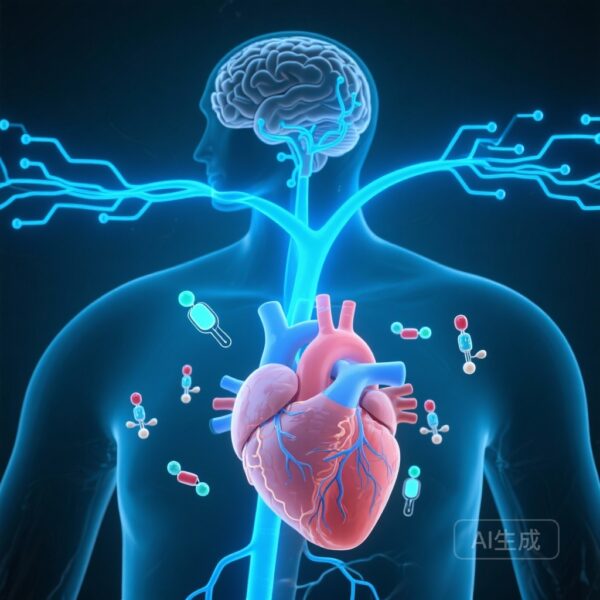
Heart failure (HF) is increasingly recognized not merely as a hemodynamic disorder but as a complex multisystem syndrome characterized by profound neurohormonal and metabolic derangements. A hallmark of HF is cardiac autonomic dysfunction, typically manifesting as a combination of sympathetic overactivity and a withdrawal of parasympathetic (vagal) tone. This autonomic imbalance is not a passive consequence of cardiac pump failure; rather, it is a primary driver of disease progression, arrhythmia risk, and mortality.
Parallel to these autonomic shifts, metabolic dysregulation—specifically insulin resistance and glucose intolerance—is highly prevalent in the heart failure population. While the link between diabetes and cardiovascular disease is well-established, the specific influence of insulin metabolism on the autonomic nervous system’s ability to regulate heart rate remains an area of intense scientific inquiry. The Myovasc study sought to bridge this gap by examining how various markers of glucose and insulin metabolism correlate with cardiac vagal activity, as reflected by heart rate recovery after exercise.
Study Design and Methodology
The Myovasc Cohort
The study utilized data from the MyoVasc study (NCT04064450), a large-scale, prospective heart failure cohort. The analysis sample included 1,588 individuals with a median age of 64.0 years. Notably, the study population reflected a clinically relevant cross-section of the HF spectrum, with 43.7% of participants presenting with symptomatic heart failure and a significant proportion exhibiting varying degrees of glucose metabolism dysfunction.
Assessment of Vagal Activity and Metabolic Markers
To quantify cardiac vagal activity, researchers employed Heart Rate Recovery at 60 seconds (HRR60) following a standardized cardiopulmonary exercise test (CPET). HRR60 is a validated surrogate for parasympathetic reactivation; a slower decline in heart rate post-exercise indicates impaired vagal tone. The metabolic assessment was comprehensive, including fasting glucose, HbA1c (long-term glycemia), HOMA-IR (insulin resistance), and C-peptide (a stable marker of endogenous insulin secretion).
The researchers utilized multivariable linear regression models, adjusting for a wide array of potential confounders, including age, sex, cardiovascular risk factors, comorbidities, and medications. A critical aspect of the methodology was the cross-adjustment between glucose markers (HbA1c) and insulin markers (HOMA-IR/C-peptide) to determine which factor was the primary driver of autonomic impairment.
Key Findings: The Primacy of Insulin Status
Cross-Sectional Associations
The initial analysis revealed that both HbA1c and HOMA-IR were significantly associated with lower HRR60. Specifically, higher HbA1c and higher HOMA-IR predicted a slower heart rate recovery. However, the most striking results emerged during the cross-adjustment models. When HOMA-IR was added to the HbA1c model, the statistical significance of HbA1c vanished (P = 0.28). Conversely, HOMA-IR remained a robust and independent predictor of HRR60 (P < 0.0001), even after adjusting for glycemic status.
This suggests that the observed link between high blood sugar and poor autonomic function is actually mediated by insulin resistance. In patients with similar glucose levels, those with higher insulin resistance exhibited significantly worse vagal reactivation.
The Role of C-Peptide
The study further identified C-peptide as a particularly potent marker. C-peptide levels were related to HRR60 independently of HbA1c, with effect estimates that exceeded those of HOMA-IR. This finding underscores the possibility that hyperinsulinemia or the biological processes associated with excessive insulin production have a direct, detrimental impact on the vagal pathways controlling the heart.
Longitudinal Analysis
The longitudinal arm of the study followed participants over two years. The results confirmed that baseline metabolic dysfunction was not just a snapshot in time. Higher baseline HbA1c and C-peptide levels were associated with lower HRR60 at the two-year mark, suggesting that metabolic derangement may contribute to a progressive decline in autonomic health over time.
Expert Commentary and Mechanistic Insights
The Myovasc study provides compelling evidence that insulin metabolism is a more critical determinant of cardiac autonomic health than simple glycemic control. From a pathophysiological perspective, several mechanisms may explain this relationship. Hyperinsulinemia is known to stimulate the sympathetic nervous system, but these findings suggest it simultaneously impairs the parasympathetic ‘brake.’ Chronic insulin resistance is also associated with systemic inflammation and oxidative stress, both of which can lead to autonomic neuropathy and impaired signaling in the vagus nerve.
For clinicians, these findings emphasize that managing heart failure requires looking beyond standard glucose targets. The independent role of insulin resistance suggests that therapies improving insulin sensitivity—such as SGLT2 inhibitors or GLP-1 receptor agonists—might offer neuro-cardiac benefits that are not captured by measuring HbA1c alone. Furthermore, the study highlights HRR60 as a simple yet powerful clinical tool to assess the integrated metabolic and autonomic health of the patient.
Conclusion
The Myovasc study clarifies the hierarchical relationship between metabolism and autonomic function in heart failure. By demonstrating that insulin resistance and secretion markers override HbA1c as predictors of cardiac vagal activity, the research shifts the focus toward the metabolic-autonomic axis. Future studies should investigate whether interventions specifically targeting insulin resistance can restore vagal tone and improve clinical outcomes in the heart failure population.
Funding and Clinical Trial Information
The MyoVasc study is registered at ClinicalTrials.gov under the identifier NCT04064450. The research was supported by various academic and clinical grants dedicated to cardiovascular and metabolic health research.
References
- Bélanger N, Zeid S, Velmeden D, et al. Cardiac vagal activity is associated with insulin metabolism in heart failure: Results from the Myovasc study. Cardiovasc Diabetol. 2026;25(1):26.
- Verrier RL, Tan A. Heart rate, heart rate variability, and heart rate recovery as risk factors and therapeutic targets. J Cardiovasc Electrophysiol. 2009;20(5):575-579.
- Sayer G, Bhat G. The relevance of insulin resistance in heart failure. J Card Fail. 2014;20(6):442-450.