Advancing Precision in Head and Neck Oncology: The Paradigm Shift
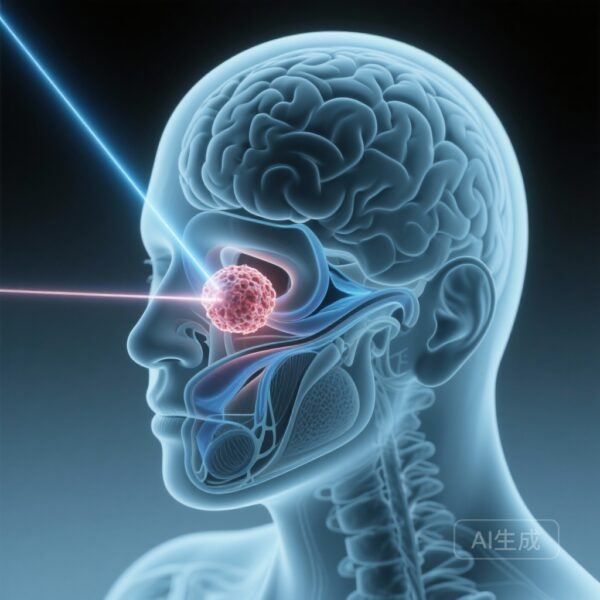
Nasopharyngeal carcinoma (NPC) presents a unique challenge in radiation oncology. Located deep within the skull base, the nasopharynx is surrounded by critical neurological and glandular structures, including the brainstem, optic nerves, temporal lobes, and salivary glands. While Intensity-Modulated Radiotherapy (IMRT) has long been the gold standard, providing excellent locoregional control, its physical properties—specifically the ‘exit dose’ of photon beams—often result in significant collateral damage to healthy tissues.
A landmark case-control study by Cao and colleagues, published in The Lancet Regional Health – Americas (2025), provides compelling evidence that Intensity-Modulated Proton Therapy (IMPT) may offer a superior therapeutic index. By leveraging the unique physical properties of protons, specifically the Bragg peak, clinicians can now deliver high-dose radiation to the tumor with virtually no dose beyond the target, potentially transforming the survivorship experience for NPC patients.
The Physical Advantage: Protons vs. Photons
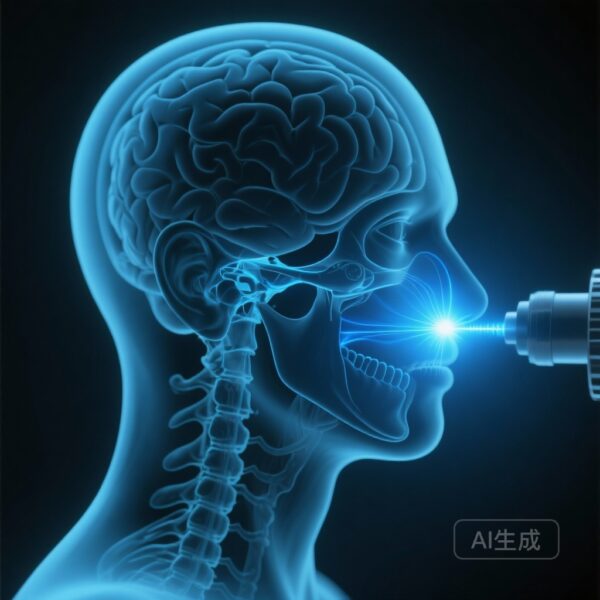
To understand the clinical significance of this study, one must first appreciate the dosimetric differences between the two modalities. Traditional IMRT utilizes megavoltage X-rays (photons), which pass through the entire body, depositing energy along the entry and exit paths. In contrast, IMPT uses heavy charged particles (protons) that can be programmed to stop at a specific depth. This lack of an exit dose allows for the ‘sparing’ of organs at risk (OARs) that are situated behind or adjacent to the tumor.
In NPC, this sparing is not merely a theoretical dosimetric exercise; it translates into the protection of the oral cavity, submandibular glands, and the posterior pharyngeal constrictor muscles. The MSKCC study sought to quantify whether these dosimetric advantages result in measurable clinical benefits during and after treatment.
Study Design and Methodology
The research conducted by Cao et al. was a rigorous case-control study involving patients treated at Memorial Sloan Kettering Cancer Center (MSKCC). The researchers compared 115 patients treated with IMPT against a matched cohort of 230 patients treated with IMRT. Matching was performed based on critical prognostic factors, including T-stage, N-stage, age, and chemotherapy use, to ensure a balanced comparison.
Primary endpoints focused on both oncologic outcomes—such as locoregional control (LRC), progression-free survival (PFS), and overall survival (OS)—and toxicity profiles, specifically the incidence of grade 2 or higher acute and late toxicities. A secondary focus was placed on the requirement for gastrostomy tube (G-tube) placement, a common surrogate for severe treatment-related morbidity in head and neck cancer.
Key Findings: Toxicity and Quality of Life
The results of the study underscore a significant clinical advantage for IMPT in terms of toxicity reduction without compromising oncologic efficacy.
Reduction in Gastrostomy Tube Dependence
One of the most striking findings was the reduction in the need for G-tubes. Patients in the IMPT group were significantly less likely to require a feeding tube during treatment compared to those in the IMRT group. This is directly attributed to the lower ‘integral dose’ delivered to the oral cavity and the pharyngeal musculature, which preserves the patient’s ability to swallow (deglutition) and maintain nutritional intake during the rigorous treatment course.
Sparing of Salivary Glands and Oral Cavity
IMPT demonstrated a superior ability to spare the contralateral parotid gland and the submandibular glands. Consequently, the incidence of grade 2+ xerostomia (chronic dry mouth) was markedly lower in the proton cohort. For survivors of NPC, chronic xerostomia is a leading cause of long-term dissatisfaction, contributing to dental decay, difficulty speaking, and impaired taste.
Neurological Sparing and Late Effects
Because NPC is often located near the skull base, radiation-induced brain injury (RIBI), particularly temporal lobe necrosis, is a feared late complication. The study observed that IMPT significantly reduced the mean dose to the temporal lobes and brainstem. While longer follow-up is always required to fully assess late neurological sequelae, the dosimetric data suggests a much lower risk profile for IMPT-treated patients.
Oncologic Outcomes: Maintaining the Standard
Crucially, the reduction in toxicity did not come at the cost of tumor control. The study reported that the 3-year locoregional control and overall survival rates were nearly identical between the two groups.
– Locoregional Control: Both cohorts achieved rates exceeding 90%.
– Overall Survival: No statistically significant difference was found, confirming that protons are at least as effective as photons in eradicating NPC.
This finding is essential for the clinical adoption of IMPT, as it reassures oncologists that the ‘softer’ treatment approach does not risk patient survival.
Expert Commentary and Clinical Implications
Dr. Nancy Lee, a senior author of the study and a leading authority in head and neck radiation oncology, has frequently emphasized that the goal of modern oncology is not just to cure, but to cure ‘well.’ The findings from this Lancet Regional Health – Americas paper suggest that IMPT is a critical tool in achieving this goal.
However, the widespread adoption of IMPT faces hurdles, primarily cost and access. Proton therapy facilities are expensive to build and operate, leading to higher treatment costs compared to IMRT. However, proponents argue that when one considers the ‘total cost of care’—including the management of toxicities, G-tube maintenance, and the treatment of late complications—IMPT may be more cost-effective than it appears on the surface.
Furthermore, the study highlights the importance of patient selection. While almost all NPC patients could benefit from the dosimetric profile of protons, those with advanced T-stage disease or tumors involving the skull base stand to gain the most.
Conclusion: A New Chapter for NPC Treatment
The case-control study by Cao et al. provides high-quality evidence that IMPT offers a superior toxicity profile compared to IMRT for nasopharyngeal carcinoma. By significantly reducing the need for feeding tubes and lowering the incidence of xerostomia, IMPT addresses the most burdensome side effects of traditional radiotherapy.
As we move forward, the focus must shift toward optimizing proton planning and expanding access to this technology. For the clinician, these results provide the necessary data to justify the use of proton therapy in NPC, particularly for patients at high risk of treatment-related morbidity. For the patient, it offers the hope of a life after cancer that is not defined by the scars of their treatment.
Funding and Trial Information
This research was supported in part by the National Institutes of Health (NIH) and National Cancer Institute (NCI) Cancer Center Support Grant (P30 CA008748). No specific clinical trial registration number was required for this retrospective case-control analysis, though it followed institutional review board (IRB) protocols at Memorial Sloan Kettering Cancer Center.
References
1. Cao C, Treechairusame T, Safavi AH, et al. Intensity-modulated proton therapy vs intensity-modulated radiotherapy in nasopharyngeal carcinoma: a case-control study. Lancet Reg Health Am. 2025;54:101352. doi:10.1016/j.lana.2025.101352.
2. Lee NY, et al. Comparative analysis of proton versus photon therapy for head and neck cancers. J Clin Oncol. 2021;39(15_suppl):6001.
3. Langendijk JA, et al. Selection of patients for radiotherapy with protons (the model-based approach). Radiother Oncol. 2018;128(1):37-47.