Highlight
1. Blood-based biomarkers (BBM) for neurodegenerative diseases vary considerably with age, genetic, metabolic, and lifestyle factors.
2. APOE ε4 carrier status and serum creatinine levels strongly associate with adverse BBM profiles in midlife and older adults.
3. Several cardiometabolic factors relate negatively with BBM, though their effects are modulated by body mass index (BMI).
4. Significant intergenerational correlations exist for phosphorylated Tau-217, GFAP, and neurofilament light chain, predominantly between mothers and offspring, but not for amyloid β42:40 ratio.
Study Background
Neurodegenerative diseases, including Alzheimer’s disease (AD) and related dementias, pose mounting public health challenges owing to aging populations globally. Early and accurate diagnosis is crucial for prognosis, management, and therapeutic interventions. While cerebrospinal fluid and neuroimaging biomarkers have been invaluable, their invasive nature and high costs limit widespread applicability. Blood-based biomarkers (BBM) have emerged as promising, cost-effective alternatives that can potentially streamline differential diagnosis and disease monitoring. However, biological variability, population-level determinants, and familial transmission patterns governing BBM remain insufficiently understood.
Study Design
The present cohort study leverages the multigenerational Young Finns Study to explore BBM distributions and determinants spanning midlife to advanced age. Participants included 1,237 middle-aged adults (41–56 years) and 814 of their parents (59–90 years). Using the Quanterix Simoa HD-X analyser, plasma concentrations of amyloid β isoforms (amyloid β42, amyloid β40), phosphorylated Tau (pTau)-217, glial fibrillary acidic protein (GFAP), and neurofilament light chain (NfL) were quantified.
A comprehensive suite of variables was analyzed for their association with BBM, encompassing demographics (age, sex), genetic factors (notably APOE ε4 carrier status), cardiometabolic measures (glucose metabolism, lipid profile), liver and kidney function markers (creatinine), and lifestyle metrics. Statistical analyses focused on quantifying individual-level predictors and estimating intergenerational correlations of BBM, emphasizing mother-offspring and father-offspring dyads.
Key Findings
Age and BBM Concentrations: Advancing age correlated strongly with unfavorable BBM profiles, reflecting increased amyloid and tau pathology markers.
Genetic Influence – APOE ε4 Status: Among parental participants, APOE ε4 carrier status robustly associated with lower amyloid β42:40 ratios (indicative of amyloid pathology), elevated pTau-217 levels, and increased GFAP, underlining genetic susceptibility’s role in biomarker changes linked to neurodegeneration.
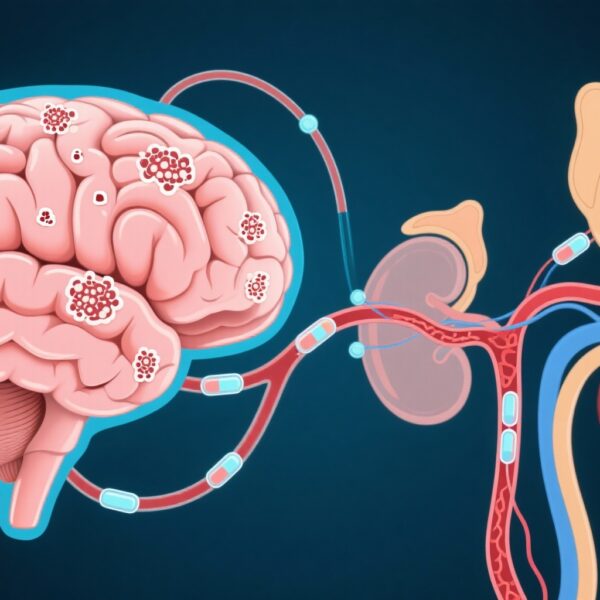
Renal Function and BBM: Higher serum creatinine emerged as a consistent adverse factor correlated with elevated pTau-217, GFAP, and NfL concentrations across generations, suggesting kidney function’s impact on biomarker clearance or systemic inflammation modulating neurodegenerative pathways.
Cardiometabolic Factors: Markers indicating glucose metabolism disturbances and dyslipidaemia showed negative associations with all examined BBM. However, these relationships were attenuated after adjusting for BMI, indicating that adiposity may mediate or confound metabolic influences on BBM.
Intergenerational Associations: Statistically significant correlations (ranging 0.20–0.33) between parents and offspring were detected for pTau-217, GFAP, and NfL, predominantly in mother-child pairs, suggesting familial transmission or shared environmental influences on neuronal injury and glial activation biomarkers. Conversely, amyloid β42:40 ratio showed no intergenerational correlation, implying distinct pathophysiological or genetic regulation mechanisms.
Expert Commentary
The study presents a comprehensive population-based evaluation of factors influencing BBM, an area pivotal to advancing blood-based diagnostics of neurodegenerative diseases. Identifying APOE ε4 carriage and serum creatinine as major influences aligns with established genetic predisposition and systemic organ function in dementia pathology. The attenuation of cardiometabolic associations after BMI adjustment underscores the complex interplay between obesity and metabolic health in modulating neurodegeneration markers.
Intergenerational correlations for pTau-217, GFAP, and NfL highlight potential maternal genetic or household-level environmental effects, warranting further mechanistic research. The absence of amyloid β42:40 ratio correlation suggests that amyloid pathology markers might be more influenced by individual lifetime exposures rather than inherited or familial factors.
Clinically, these findings caution that BBM interpretation must consider extrinsic physiological factors beyond primary neuropathology to avoid misclassification. Future investigations should aim to delineate which BBM variations directly reflect neurodegenerative cascades versus systemic or metabolic effects to refine biomarker-based diagnostic criteria.
Conclusion
This cohort study elucidates multifactorial determinants influencing BBM related to neurodegenerative disease including genetic, metabolic, renal, and intergenerational components. Awareness of these factors is essential to enhance the clinical utility, reliability, and interpretation of blood biomarkers in dementia diagnostics and research. Incorporating such insights advances personalized medicine approaches and may improve early disease detection and monitoring in broader populations.
Funding
The Young Finns Study cohort research received extensive support from Finnish research councils, hospital research funding, foundations related to cardiovascular and neurological diseases, and European funding bodies including the EU Horizon 2020 and European Research Council.
Reference
Heiskanen MA, Mykkänen J, Pahkala K, et al. Factors related to blood-based biomarkers for neurodegenerative diseases and their intergenerational associations in the Young Finns Study: a cohort study. Lancet Healthy Longev. 2025 Jun;6(6):100717. doi: 10.1016/j.lanhl.2025.100717. PMID: 40645733; PMCID: PMC12242518.