Highlight
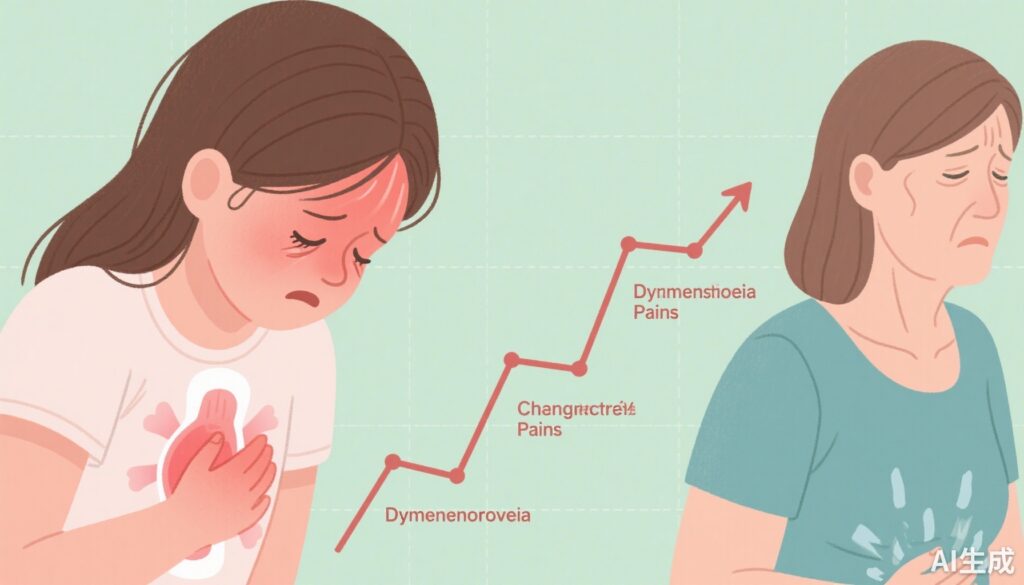
• Moderate to severe dysmenorrhoea at age 15 is associated with a 65-76% increased risk of chronic pain by age 26.
• Approximately 60% of adolescents in the cohort reported moderate or severe dysmenorrhoea.
• Anxiety and depressive symptoms partially mediate the association between severe dysmenorrhoea and chronic pain.
• Early recognition and management of adolescent dysmenorrhoea represent a critical public health opportunity.
Study Background
Dysmenorrhoea, defined as painful menstrual cramps of uterine origin, affects a substantial proportion of adolescent girls worldwide and is a leading cause of menstrual-related disability. Despite its high prevalence, dysmenorrhoea is often underdiagnosed and undertreated due to sociocultural stigma and misconceptions about menstruation. Emerging evidence indicates that dysmenorrhoea rarely occurs in isolation and frequently coexists with other chronic pain conditions. Additionally, adult women with dysmenorrhoea demonstrate increased sensory sensitivity, suggesting potential alterations in pain processing mechanisms.
Understanding whether dysmenorrhoea in adolescence predisposes individuals to chronic pain in later life is vital to identifying at-risk populations and informing preventive strategies. Chronic pain itself represents a significant healthcare burden with profound impacts on quality of life, functionality, and mental health. This longitudinal study leverages a large UK birth cohort to investigate the temporal relationship between adolescent dysmenorrhoea and subsequent chronic pain outcomes.
Study Design
The research utilized data from the Avon Longitudinal Study of Parents and Children (ALSPAC), a well-established UK population-based birth cohort initiated with mothers expected to deliver between April 1991 and December 1992. Annual self-reports of dysmenorrhoea were collected from participants aged 8 to 17 years, with severity at age 15 categorized as none, mild, moderate, or severe.
At age 26, participants reported any aches or pains lasting one day or longer in the past month, and whether pain duration met the threshold for chronicity (≥3 months). Participants with pre-existing pain conditions before menarche or only acute pain were excluded to isolate the impact of adolescent dysmenorrhoea on new-onset chronic pain in adulthood.
Multivariable logistic regression models adjusted for multiple confounders associated with both dysmenorrhoea and chronic pain, including ethnicity, maternal education, early life adversity, pre-menarche depressive symptoms, physical activity, smoking, polyunsaturated fatty acid intake, and body mass index at menarche. Multiple imputation addressed missing data. Anxiety and depressive symptoms following dysmenorrhoea reporting were evaluated as potential mediators using bootstrapping techniques.
Key Findings
The analytic sample included 1157 participants, of whom 691 (59.7%) reported moderate or severe dysmenorrhoea at age 15. By age 26, 307 (26.5%) reported chronic pain. Stratified by dysmenorrhoea severity at 15, chronic pain prevalence was 17.3% (no dysmenorrhoea), 22.1% (mild), 30.0% (moderate), and 33.5% (severe).
Adjusted relative risks (RR) for chronic pain at age 26 compared with no dysmenorrhoea were:
- Mild: RR 1.23 (95% CI 0.85-1.74; p=0.27)
- Moderate: RR 1.65 (1.22-2.18; p=0.0021)
- Severe: RR 1.76 (1.23-2.39; p=0.0030)
The corresponding absolute risk increases were 4.8, 12.7, and 16.2 percentage points for mild, moderate, and severe dysmenorrhoea, respectively.
Mediation analyses revealed that anxiety and depressive symptoms shortly after dysmenorrhoea diagnosis accounted for a small but notable portion of the increased risk of chronic pain, particularly in severe cases. This suggests psychological comorbidities partially contribute to the long-term pain burden.
Expert Commentary
This study compellingly links adolescent dysmenorrhoea with an elevated risk of chronic pain in early adulthood, using a robust prospective design that adjusts for a wide range of confounders. The dose-response relationship strengthens causal inference. By excluding participants with prior pain conditions, the analysis isolates dysmenorrhoea as a potential independent risk factor rather than a marker of existing pain vulnerability.
Mechanistically, dysmenorrhoea may induce central sensitization through repeated nociceptive input during adolescence, a critical neurodevelopmental window for pain processing. Increased sensory sensitivity in affected adults supports this hypothesis. The partial mediation by mood symptoms aligns with biopsychosocial models of chronic pain and highlights the importance of holistic assessment and intervention.
Limitations include reliance on self-reported pain outcomes, which may introduce reporting bias, and the UK-centric cohort, which might limit generalizability to ethnically or culturally diverse populations. Nevertheless, the findings resonate with international clinical observations of overlapping pain syndromes and menstrual-related disorders.
Conclusion
The study pioneers longitudinal evidence that dysmenorrhoea in adolescence is more than an acute menstrual complaint; it poses a significant risk factor for chronic pain development into adulthood. These findings underscore the urgent need for improved recognition, diagnosis, and management of dysmenorrhoea in young girls. Early interventions, encompassing both pharmacological and non-pharmacological strategies, may mitigate the trajectory towards chronic pain.
Importantly, the role of menstrual literacy and destigmatization cannot be overstated to empower adolescents and caregivers in timely healthcare engagement. Further research should explore targeted prevention approaches, including addressing psychological factors and elucidating the pathophysiology linking dysmenorrhoea to chronic pain syndromes.
Funding and Trial Registration
This work was funded by the UK Research and Innovation Strategic Priorities Fund Advanced Pain Discovery Platform, supported by UK Medical Research Council, Biotechnology and Biological Sciences Research Council, Economic and Social Research Council, Versus Arthritis, the Medical Research Foundation, and Eli Lilly and Company.
References
- Reid-McCann R, Poli-Neto OB, Stein K, et al. Longitudinal association between dysmenorrhoea in adolescence and chronic pain in adulthood: a UK population-based study. Lancet Child Adolesc Health. 2025 Nov;9(11):766-775. doi:10.1016/S2352-4642(25)00213-5.
- Burnett M, Lemyre M. Dysmenorrhea severity and menstrual coping in adolescent girls: a population-based study. J Adolesc Health. 2017;60(2):214-220.
- LeResche L. Pain and menstrual cycle. Pain. 1997;73(1):1-4.
- Vincent K, Becker CM, Grimes T, et al. Sensory sensitivity and chronic pelvic pain: evidence for central sensitization in endometriosis and primary dysmenorrhoea. Br J Pain. 2020;14(4):245-256.