Highlight
- An AI-driven imaging pipeline was developed to automatically segment lymph nodes and classify extranodal extension (iENE) on pretreatment CT scans in HPV-positive oropharyngeal carcinoma (OPC).
- The AI model achieved high accuracy (AUC 0.81) in detecting iENE compared to evaluations by expert neuroradiologists, addressing limitations of subjective imaging interpretation.
- AI-predicted iENE was independently associated with worse overall survival, recurrence-free survival, and distant control, outperforming radiologist assessments in prognostic discrimination.
- This approach offers a reproducible, scalable tool for risk stratification in HPV-positive OPC, highlighting the potential of AI to enhance personalized treatment planning.
Study Background
Oropharyngeal carcinoma (OPC) related to human papillomavirus (HPV) infection represents a distinct clinical and biological entity with generally favorable prognosis compared to HPV-negative counterparts. Despite this, the presence of extranodal extension (ENE)—the spread of cancer beyond the lymph node capsule—is a well-recognized adverse prognostic factor in head and neck cancers. Particularly in HPV-positive OPC, imaging-based detection of extranodal extension (iENE) from pretreatment scans has been linked to worse clinical outcomes. However, iENE is currently not included in the eighth edition of the American Joint Committee on Cancer (AJCC) staging system for HPV-related OPC, partly due to challenges including lack of standardized imaging criteria, dependence on radiologic expertise, and interobserver variability. To improve prognostication and risk stratification, more objective and reproducible methods to detect iENE are needed.
Study Design
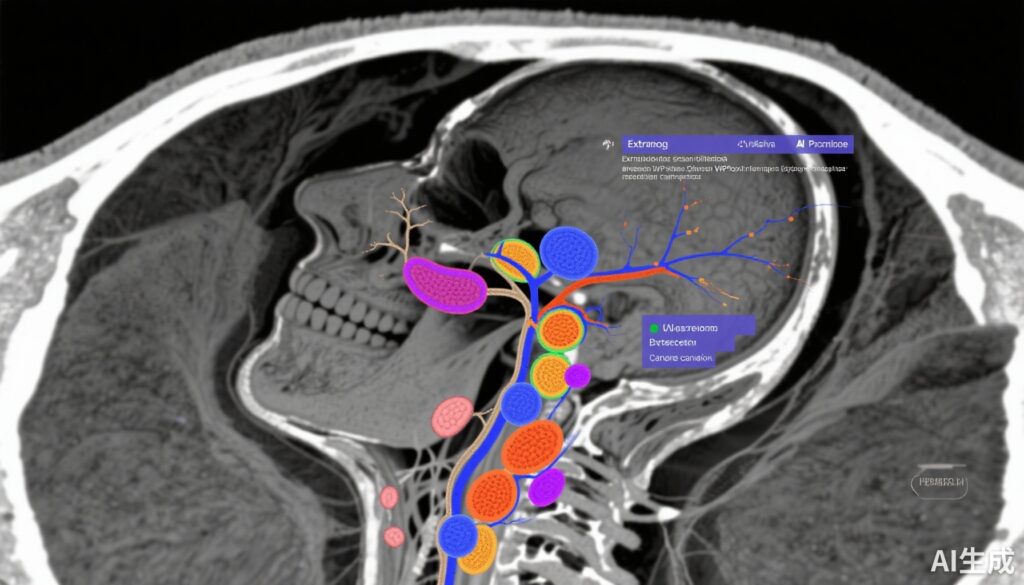
This single-center cohort study was conducted at a tertiary oncology center in Montreal, Canada. Adult patients with HPV-positive clinically node-positive (cN+) oropharyngeal carcinoma who received upfront (chemo)radiotherapy between January 2009 and January 2020 were included. Participants were followed through January 2024. Pretreatment planning computed tomography (CT) scans were sourced, and expert radiation oncologists provided lymph node gross tumor volume segmentations as the reference standard.
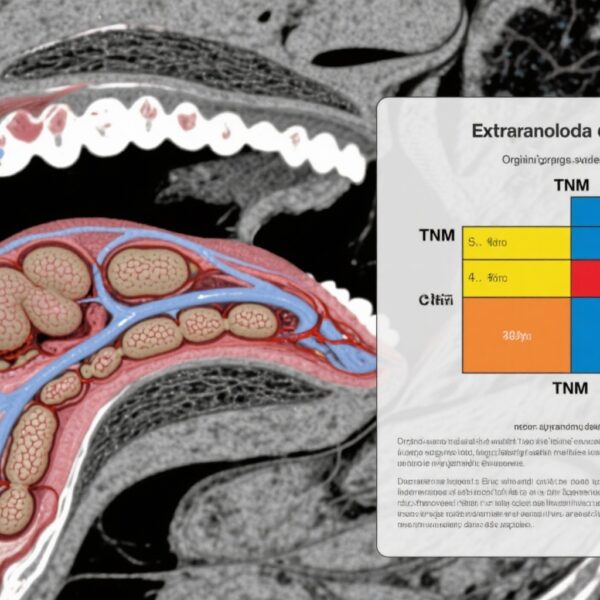
For lymph node segmentation, the study developed an nnU-Net deep learning model, a robust and adaptable convolutional neural network framework optimized for medical image segmentation. For classification of iENE, the pipeline compared radiomic feature extraction—quantitative imaging features reflecting shape, texture, and intensity—with deep learning approaches to ascertain the optimal method for predicting extranodal extension.
Primary outcome measures included classification accuracy of AI-predicted iENE compared to consensus expert neuroradiologist evaluations, quantified by area under the receiver operating characteristic curve (AUC). Subsequently, the association between AI-predicted iENE and oncologic outcomes was analyzed, focusing on overall survival (OS), recurrence-free survival (RFS), distant control (DC), and locoregional control (LRC).
Key Findings
Among 397 patients (mean age 62.3 years; 80 females and 317 males), the AI-based model utilizing radiomic features achieved an AUC of 0.81 for iENE classification, demonstrating good discriminatory power. Importantly, patients with AI-predicted iENE had significantly poorer 3-year outcomes: OS was 83.8% compared with 96.8% in AI-negative cases; RFS was 80.7% vs 93.7%; and DC was 84.3% vs 97.1%. Locoregional control did not show significant difference.
The AI model outperformed expert neuroradiologist assessments in prognostic discrimination, with higher concordance indices for OS (0.64 vs 0.55), RFS (0.67 vs 0.60), and DC (0.79 vs 0.68). Multivariable regression adjusting for known confounders—age, tumor category, nodal category, and number of involved lymph nodes—affirmed that AI-predicted iENE remained an independent predictor of worse survival outcomes: adjusted hazard ratios (aHR) were 2.82 for OS, 4.20 for RFS, and 12.33 for DC.
These results indicate that the AI algorithm not only identifies imaging features correlating with ENE presence but also translates these findings into meaningful clinical outcome prediction.
Expert Commentary
This study pioneers the integration of artificial intelligence in the nuanced imaging-based assessment of extranodal extension in HPV-related OPC. By automating lymph node segmentation and feature extraction, the approach reduces inter-reader variability, a major limitation previously encountered in imaging interpretation for ENE. The high prognostic value of AI-predicted iENE suggests that it could become a critical biomarker to further refine risk stratification and tailor treatment intensities.
Nevertheless, this study is limited by its single-institution design, which may restrict the generalizability of findings. Variability in CT acquisition protocols between centers and demographic heterogeneity underline the need for external validation studies. Moreover, while radiomic analysis outperformed deep learning in this study for iENE classification, the combination of these approaches or incorporation of multimodal imaging could enhance diagnostic performance.
Current guidelines do not incorporate imaging-based ENE in staging or treatment decision algorithms for HPV-positive OPC. If externally validated, AI-driven iENE detection could influence clinical workflows, potentially guiding more aggressive therapy or adjuvant treatment considerations in patients deemed high risk. This highlights an evolving role for AI tools in personalized oncology.
Future research should address prospective validation, integration with other biomarkers including molecular and histopathological data, and real-world implementation feasibility, especially in centers with limited radiologic expertise.
Conclusion
This study demonstrates that an AI-driven pipeline using pretreatment CT scans can reliably detect imaging-based extranodal extension in HPV-positive oropharyngeal cancer and independently predict worse oncologic outcomes. The model surpasses expert neuroradiologist assessments in prognostic accuracy, offering a scalable solution to an important clinical challenge. Adoption of such AI tools could refine patient risk profiling and influence individualized treatment strategies. However, external validation and assessment across diverse clinical settings are essential before widespread clinical implementation.
Funding and ClinicalTrials.gov
The original study did not specify funding sources or clinical trial registration details within the provided content. Further reference to original publication may clarify these aspects.
References
Dayan GS, Hénique G, Bahig H, Nelson K, Brodeur C, Christopoulos A, Filion E, Nguyen-Tan PF, O’Sullivan B, Ayad T, Bissada E, Tabet P, Guertin L, Desilets A, Kadoury S, Letourneau-Guillon L. Artificial Intelligence Model for Imaging-Based Extranodal Extension Detection and Outcome Prediction in Human Papillomavirus-Positive Oropharyngeal Cancer. JAMA Otolaryngol Head Neck Surg. 2025 Sep 30:e253225. doi: 10.1001/jamaoto.2025.3225. Epub ahead of print. PMID: 41026592; PMCID: PMC12486138.