Background
Cirrhotic portal hypertension (CPH) is a severe complication of liver cirrhosis characterized by increased portal vein pressure leading to significant morbidity and mortality worldwide. While clinical management of CPH traditionally focuses on hemodynamic and liver function parameters, emerging evidence implicates gut microbiota— the complex community of microorganisms residing in the gastrointestinal tract — as a critical contributor to liver disease progression. Alterations in gut microbiota composition and function, commonly described as dysbiosis, have been associated with systemic inflammation, endotoxemia, and immune dysregulation in chronic liver diseases. However, the specific role of gut microbiota in the pathophysiology and progression of CPH remains insufficiently understood.
Study Design and Methods
In a recent study by Zhang et al. (2025), gut microbial and metabolic profiles were comprehensively evaluated in 106 participants comprising 35 patients diagnosed with cirrhotic portal hypertension and 71 control patients without CPH. Faecal samples were subjected to microbiome (16S rRNA sequencing and metagenomic analyses) and metabolomic assessments to delineate the structural and functional alterations associated with CPH.
To investigate causal relationships, the research team employed in vivo murine models including fecal microbiota transplantation (FMT) from human donors, transplantation of specific CPH-characteristic bacteria (Veillonella nakazawae), and antibiotic treatment interventions, alongside chemically induced CPH via N-dimethylnitrosamine (DEN) administration.
Key Findings
1. Microbial Diversity and Composition Changes: Patients with CPH demonstrated significantly diminished gut microbial diversity compared to controls, a hallmark of dysbiosis.
2. Enrichment of Pathogenic Taxa and Loss of Protective Bacteria: Notably, there was an increased abundance of lipopolysaccharide (LPS)-producing bacteria, which can exacerbate systemic inflammation through endotoxin release, coupled with a reduction in anti-inflammatory and homeostasis-maintaining microbial populations.
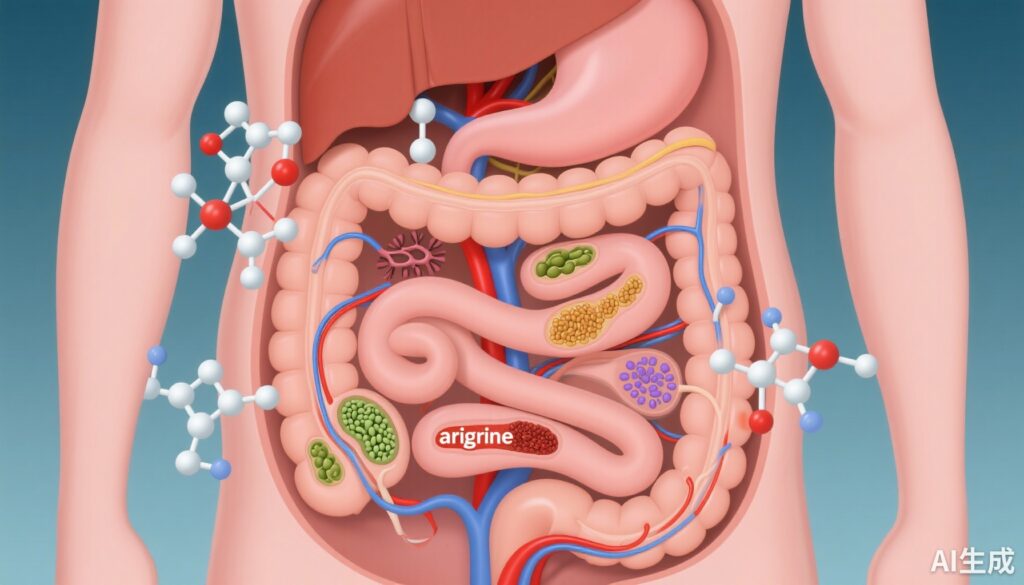
3. Metabolic Alterations: Metabolomic profiling revealed perturbed faecal metabolite patterns, with significant disruptions in arginine biosynthesis and nitric oxide (NO) production pathways. These metabolic changes are mechanistically relevant since NO is a critical vasodilator involved in regulating portal vein resistance and blood flow.
4. Functional Implications in Disease Progression: Transferring the gut microbiota from CPH patients into murine models aggravated portal hypertension and related pathological parameters. Additionally, targeted transplantation of Veillonella nakazawae, identified as a CPH-associated opportunistic species, exacerbated disease features.
5. Therapeutic Potential of Antibiotic Intervention: Administration of antibiotics in the DEN-induced CPH mouse model significantly alleviated portal pressure elevation and inflammatory markers, indicating that microbiota modulation can beneficially influence CPH progression.
Expert Commentary
This study provides compelling evidence that dysbiosis, characterized by a loss of microbial diversity and an abundance of pro-inflammatory bacteria, contributes directly to the pathogenesis and progression of cirrhotic portal hypertension. The observed imbalances in arginine and nitric oxide metabolism further link the gut microbial ecosystem to vascular and inflammatory alterations critical in CPH.
Mechanistically, increased LPS-producing bacteria may promote systemic endotoxemia, heightening liver inflammation and fibrotic progression that exacerbate portal hypertension. The identification of Veillonella nakazawae as a pathogenic mediator introduces a potential microbiological target for therapeutic intervention.
However, the study’s findings should be interpreted considering certain limitations, including the relatively small sample size and the complexity of human microbiota that may limit direct clinical translation. Future studies must elucidate precise microbial mechanisms and evaluate microbiome-directed therapies, such as probiotics, prebiotics, or selective antibiotics, in larger clinical cohorts.
Conclusion
The comprehensive approach adopted by Zhang et al. reveals that gut microbiota alterations are intricately linked to the progression of cirrhotic portal hypertension through modulation of inflammatory and metabolic pathways. These insights not only enhance understanding of CPH pathophysiology but also highlight the gut microbiome as a promising therapeutic target. Personalized microbiome interventions might emerge as adjunct strategies to conventional treatments to alleviate portal hypertension and improve outcomes in patients with cirrhosis.
References
Zhang Q, Cui J, Hou Y, et al. Alterations in Gut Microbiota and Metabolism in Cirrhotic Portal Hypertension: Implications for Disease Progression. Aliment Pharmacol Ther. 2025 Oct 2. doi: 10.1111/apt.70392. Epub ahead of print. PMID: 41035378.
Albillos A, de Gottardi A, Rescigno M. The gut-liver axis in liver disease: Pathophysiological basis for therapy. J Hepatol. 2020;72(3):558-577.
Tripathi A, Debelius J, Brenner DA, et al. The gut-liver axis and the intersection with the microbiome. Nat Rev Gastroenterol Hepatol. 2018;15(7):397-411.
Wiest R, Lawson M, Geuking M. Pathological bacterial translocation in liver cirrhosis. J Hepatol. 2014;60(1):197-209.