Highlights
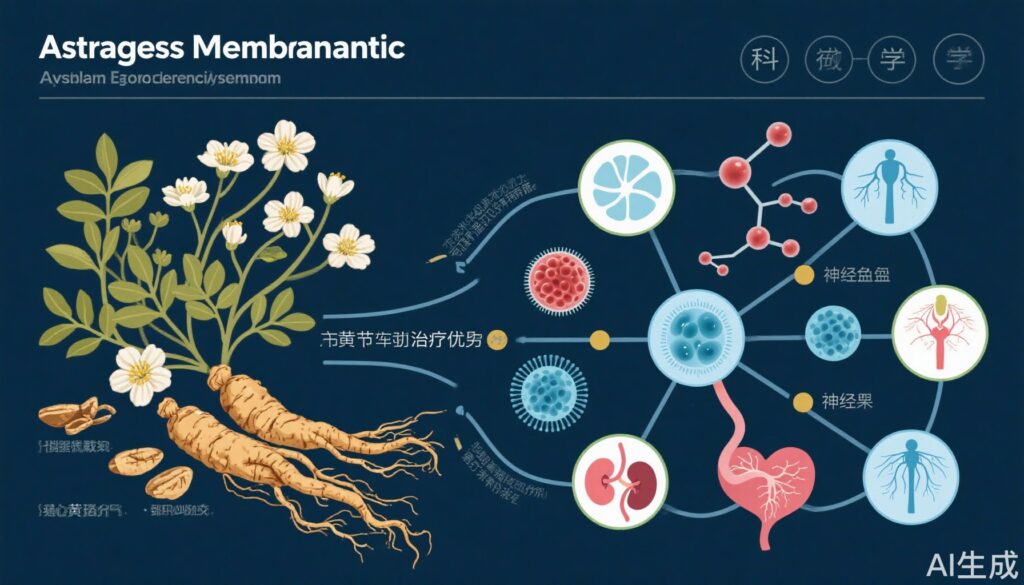
- Astragalus membranaceus (AM) exhibits broad therapeutic efficacy across chronic kidney disease, heart failure, diabetic complications, and chemotherapy-induced toxicities.
- Strong evidence supports AM’s immunomodulatory effects, with reductions in proinflammatory cytokines and improvement in cellular immunity markers.
- Combination therapy of AM with renin-angiotensin-aldosterone system (RAAS) blockers or other Western medicines significantly enhances clinical outcomes, particularly in diabetic nephropathy and membranous nephropathy.
- Network pharmacology and mechanistic studies reveal multi-target, multi-pathway actions, involving inflammatory modulation, fibrosis attenuation, oxidative stress reduction, and angiogenesis promotion.
Background
Astragalus membranaceus (huang qi), a cornerstone of Traditional Chinese Medicine (TCM), has been extensively employed due to its immunomodulatory, antioxidative, and organ-protective properties. Chronic diseases such as diabetic kidney disease (DKD), heart failure with reduced ejection fraction (HFrEF), idiopathic membranous nephropathy (IMN), and chemotherapy-induced toxicities remain clinical challenges worldwide. Conventional therapies often yield incomplete responses or significant adverse effects. Thus, exploring adjunctive herbal interventions, including AM, offers promising directions to augment efficacy and safety.
Key Content
Chronological Development and Clinical Evidence
Recent meta-analyses and systematic reviews (2021–2024) have amassed evidence supporting Astragalus membranaceus across multiple disease domains.
Diabetic Kidney Disease and Nephropathy:
– Meta-analyses involving thousands of patients demonstrate that AM, combined with RAAS blockers or TCM herbs like Rhizoma Dioscoreae, significantly reduces proteinuria, serum creatinine (SCr), blood urea nitrogen (BUN), and glycated hemoglobin (HbA1c) levels, enhancing total effective response rates (Ren Fail 2024; Altern Ther Health Med 2023).
– Animal studies confirm AM’s capacity to attenuate renal fibrosis, inflammatory cytokines (e.g., TGF-β1, CTGF), and oxidative stress markers, suggesting modulation of HIF, VEGF, and TNF signaling pathways in DKD (Phytomedicine 2024).
– Network pharmacology identified 17 active compounds targeting inflammatory responses and angiogenesis, implicating microRNA regulation (Medicine [Baltimore] 2022).
Heart Failure with Reduced Ejection Fraction (HFrEF):
– Nineteen randomized controlled trials (RCTs) encompassing 1,565 patients reveal that adjunctive AM therapy improves left ventricular ejection fraction (LVEF), reduces left ventricular end-diastolic and end-systolic diameters, and lowers natriuretic peptide levels without added adverse effects (Front Pharmacol 2024).
– Preclinical studies corroborate AM’s antifibrotic and anti-apoptotic effects and highlight its modulation of post-myocardial infarction immunohistological dynamics (Medicina 2024).
Idiopathic Membranous Nephropathy (IMN):
– Meta-analyses including over 3,400 participants indicate that AM combined with immunosuppressive or supportive therapy significantly improves remission rates and renal function indices compared to standard care alone (Medicine [Baltimore] 2023; Front Pharmacol 2022).
Diabetic Retinopathy and Chemotherapy-Induced Toxicities:
– Compounded herbal formulations with AM, such as Qiming granules, show efficacy in diabetic retinopathy through multi-target mechanisms involving vascular and inflammatory pathways (J Ethnopharmacol 2023).
– AM-containing traditional formulas reduce the incidence and severity of oxaliplatin-induced peripheral neurotoxicity and chemotherapy-induced gastrointestinal toxicity in colorectal cancer patients, improving treatment tolerability and response rates (J Ethnopharmacol 2024; Front Oncol 2021).
Immunomodulation and Mechanistic Insights
– A meta-analysis of 19 human studies encompassing 1,094 participants demonstrates that AM significantly suppresses humoral proinflammatory cytokines (IL-2, IL-4, IL-6, IL-10, TNF-α, IFN-γ) and enhances cellular immunity markers such as CD3 and CD4/CD8 ratios, underscoring its dual immunomodulatory activity (Complement Med Res 2023).
– Network pharmacology and molecular docking studies reveal that AM acts via multiple signaling pathways including JAK-STAT, VEGF, tumor necrosis factor, and chemokine pathways to alleviate inflammation, oxidative stress, and fibrosis across target organs (Heart Lung 2025; J Ethnopharmacol 2021).
Combination Therapies and Synergistic Potential
– Astragalus membranaceus combined with RAAS blockers yields superior outcomes in stage III diabetic nephropathy, including reduced proteinuria, serum creatinine, and improved glycemic control compared to monotherapy (Ren Fail 2024).
– AM combined with immunosuppressive therapies enhances remission rates in IMN and reduces proteinuria and serum creatinine levels (Medicine [Baltimore] 2023).
– Herbal formulae incorporating AM alongside other TCM herbs (e.g., Ligusticum chuanxiong, Poria cocos, Codonopsis pilosula) demonstrate additive effects in chronic pulmonary heart disease, neurotoxicity prevention, and cardiovascular diseases by targeting inflammation and oxidative stress (Heart Lung 2025; J Ethnopharmacol 2024; J Ethnopharmacol 2021).
Safety and Adverse Events
– Across multiple RCTs and meta-analyses, AM adjunctive treatments did not significantly increase adverse reactions, indicating a favorable safety profile in combination with conventional treatments (Front Pharmacol 2024; Ren Fail 2024).
Expert Commentary
The convergent evidence from clinical trials, meta-analyses, and mechanistic studies robustly supports the clinical potential of Astragalus membranaceus as an adjunct in managing chronic conditions characterized by inflammation, oxidative injury, and immune dysregulation. The immunomodulatory effects, including suppression of proinflammatory cytokines and enhancement of cellular immunity, provide a plausible biological rationale for its broad therapeutic applications.
However, limitations include heterogeneity in study designs, herbal formulations, dosages, and study quality that necessitate cautious interpretation. Notably, many clinical trials lack double-blinding and have small sample sizes, underscoring the need for large-scale, well-designed, high-quality randomized controlled trials to firmly establish efficacy and safety.
Combination therapy using AM with RAAS blockers or immunosuppressive agents offers a promising strategy, particularly in diabetic nephropathy and membranous nephropathy, amplifying therapeutic benefits synergistically.
Mechanistic insights emphasize AM’s multi-component, multi-target engagement, characteristic of herbal medicines, which may be leveraged to modulate the complex pathophysiology of chronic diseases. The modulation of microRNAs and key signaling pathways opens avenues for personalized therapies and biomarker-guided interventions.
Future research directions include pharmacokinetic studies to optimize dosing, exploration of AM in emerging indications such as chronic pulmonary heart disease and neuroprotection in chemo-induced toxicity, and integration of multi-omics approaches to decipher the holistic effects.
Conclusion
Astragalus membranaceus has demonstrated significant advances in research supporting its immunomodulatory, renal-protective, and cardioprotective effects with evidence from in vitro, animal, and human clinical studies. Its synergistic potential with conventional drugs enhances therapeutic outcomes in diabetic nephropathy, membranous nephropathy, heart failure, and chemotherapy-induced toxicities.
While AM’s safety and multimodal mechanisms are encouraging, there remain gaps necessitating more rigorous randomized trials, standardization of herbal preparations, and mechanistic elucidation. The strong tradition of AM use, combined with contemporary research findings, positions it as a valuable candidate for integration into multimodal management strategies for chronic inflammatory and degenerative diseases.
References
- Wang, J. et al. Treating chronic pulmonary heart disease with traditional Chinese medicine: Systematic evaluation and mechanistic insights (Heart Lung 2025; PMID: 39378530).
- Vargas-Sánchez, K. et al. Potential Effects of Bioactive Compounds in Chronic Kidney Disease and Dialysis: Systematic Review (Nutrients 2024; PMID: 39770942).
- Zhao, Y. et al. Efficacy of Astragalus combined with RAAS blockers for Stage III Diabetic Nephropathy (Ren Fail 2024; PMID: 38836372).
- Smith, L. et al. Preclinical studies of herbal medicines in post-myocardial infarction heart failure (Medicina 2024; PMID: 39064530).
- Chen, Y. et al. Renal protective effects and mechanisms of Astragalus (Phytomedicine 2024; PMID: 38733903).
- Lin, R. et al. Prevention of oxaliplatin-induced neurotoxicity with traditional plant-based medicines (J Ethnopharmacol 2024; PMID: 38211824).
- Li, S. et al. Astragalus membranaceus on left ventricular remodeling in HFrEF: Systematic review and meta-analysis (Front Pharmacol 2024; PMID: 38283626).
- Ma, H. et al. Astragalus and Chinese Yam combination for diabetic nephropathy (Altern Ther Health Med 2023; PMID: 37856796).
- Wang, Q. et al. Astragalus membranaceus formula for moderate-high risk idiopathic membranous nephropathy (Medicine 2023; PMID: 36862887).
- Zhang, W. et al. Pharmacological mechanism and clinical study of Qiming granules in diabetic retinopathy (J Ethnopharmacol 2023; PMID: 36332761).
- Li, J. et al. Immunomodulatory effects of Astragalus: Systematic review and meta-analysis (Complement Med Res 2023; PMID: 37952511).
- Yang, Z. et al. Advances in clinical diagnosis and pharmacotherapy of membranous nephropathy including Astragalus applications (Front Pharmacol 2022; PMID: 35694252).
- Guo, X. et al. Efficacy of Huangqi Injection in hypertensive nephropathy (Front Med 2022; PMID: 35547210).
- Wang, X. et al. Network pharmacology analysis of miRNA expression in AM treatment of diabetic nephropathy (Medicine 2022; PMID: 35119030).
- Zhao, Y. et al. Zhilong Huoxue Tongyu capsule in cardiovascular and cerebrovascular diseases with AM (J Ethnopharmacol 2021; PMID: 34044079).
- Kaczmarczyk, M. et al. AM supplementation modulates immune response to strenuous exercise (J Int Soc Sports Nutr 2021; PMID: 34271953).
- Liu, Y. et al. Herbal medicine interventions for chemotherapy-induced gastrointestinal toxicity including AM (Front Oncol 2021; PMID: 33869014).
- Zhao, X. et al. Quality and pharmacological research on Fufang Xueshuantong Capsule including AM (J Ethnopharmacol 2021; PMID: 33068651).