Introduction
Atrial fibrillation (AF) remains the most prevalent cardiac arrhythmia worldwide, contributing to significant morbidity and mortality through its association with stroke, heart failure, and sudden cardiac death. In intensive care units (ICUs), AF incidence is notably high, reported at approximately 15.6%, and is linked with worsening clinical outcomes. Given the complexity of critically ill patients, prognostication in AF remains challenging, necessitating novel and practical biomarkers for risk stratification.
Insulin resistance (IR) is a pathophysiological state implicated in metabolic syndrome and type 2 diabetes mellitus, and it correlates with cardiovascular stiffening and dysfunction. The triglyceride-glucose (TyG) index, calculated using fasting triglyceride and glucose levels, serves as a validated, cost-effective surrogate marker of IR. In the general population, elevated TyG index levels have been associated with adverse cardiovascular outcomes, including AF. However, critically ill patients experience physiological stress that can induce dynamic fluctuations in metabolic parameters, limiting the predictive value of single-point TyG measurements.
Dynamic assessment of the TyG index trajectory may better capture the temporal variations in insulin resistance during critical illness. Despite emerging evidence linking glucose variability to mortality in ICU populations, little is known about the prognostic implications of TyG index trajectories specifically in critically ill AF patients. This gap motivated the current retrospective cohort study employing group-based trajectory modeling (GBTM) to elucidate the association between distinct TyG index patterns and all-cause mortality at multiple follow-up intervals.
Study Design
This retrospective analysis utilized the publicly available MIMIC-IV database, encompassing detailed electronic health records of ICU admissions from Beth Israel Deaconess Medical Center between 2008 and 2022. Adult patients (≥18 years) with a documented diagnosis of AF on ICU admission and ICU length of stay exceeding 72 hours were included to ensure sufficient repeated measurements of glucose and triglycerides for trajectory modeling.
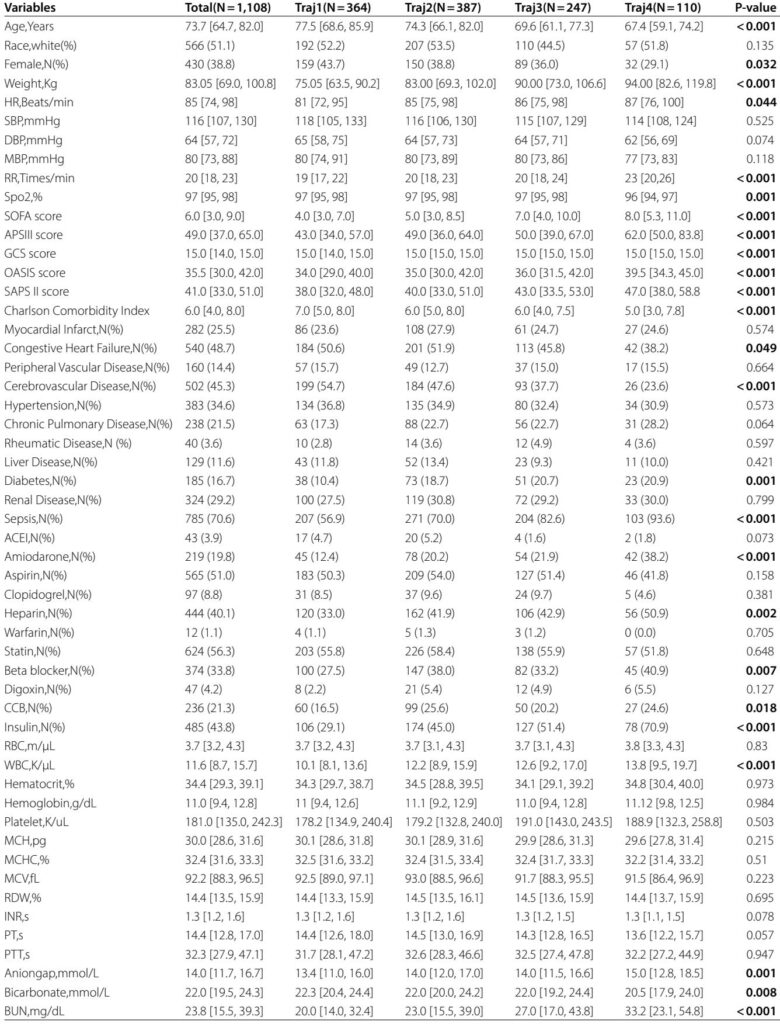
Exclusion criteria comprised insufficient laboratory data (less than three triglyceride or glucose measurements), malignancy, and multiple ICU admissions beyond the first. The final cohort consisted of 1,108 patients. Baseline demographics, comorbidities, vital signs, scores of illness severity (SOFA, SAPS II), medication use, and laboratory values were extracted. The primary outcomes were all-cause mortality at 30, 90, 180, and 365 days post-ICU admission.
The TyG index was calculated as ln [fasting triglycerides (mg/dL) × fasting glucose (mg/dL) / 2]. Using GBTM statistical methodology, patients were clustered into four distinct TyG trajectory groups based on serial measurements during ICU stay:
- traj1: Stable low TyG levels
- traj2: Slowly ascending moderate TyG
- traj3: Ascending then descending moderate-high TyG
- traj4: High-level fluctuating TyG
Survival analyses utilized Kaplan–Meier curves and Cox proportional hazards regression adjusting for relevant confounders.
Key Findings
Four TyG trajectory groups were identified, comprising 31.2%, 35.7%, 23.1%, and 10.0% of the sample respectively. Patients with fluctuating high TyG index (traj4) were younger, heavier, more frequently diabetic, had higher sepsis rates, and displayed higher severity of illness scores.
Kaplan–Meier analysis revealed that traj4 patients exhibited significantly worse survival across all follow-up points (30-, 90-, 180-, 365-day mortality) compared to patients in other trajectory groups. Adjusted Cox models confirmed that after controlling for demographic, clinical, and laboratory confounders, traj4 membership was independently associated with increased hazard ratios (HRs) for mortality at 30 days (HR=1.71, 95% CI: 1.14–2.56), 90 days (HR=1.67, 95% CI: 1.17–2.39), 180 days (HR=1.44, 95% CI: 1.03–2.06), and 365 days (HR=1.44, 95% CI: 1.04–1.98) relative to the stable low TyG group (traj1). Other trajectories did not demonstrate significant mortality differences compared to traj1.
Restricted cubic spline models suggested a linear association between elevated TyG index and increasing mortality risk. Subgroup analyses indicated the prognostic relevance of the fluctuating high TyG pattern persisted across age, sex, race, and comorbidity strata, although stronger effects were observed among males, elderly patients, non-diabetics, and statin users.
Expert Commentary
This study harnesses advanced trajectory modeling to overcome the limitations of single-point biomarkers in a heterogeneous ICU population with AF. The findings highlight that not just elevated TyG levels, but their dynamic fluctuations, portend worse prognosis. Mechanistically, fluctuations in glucose and triglycerides may stimulate oxidative stress, inflammatory cytokines, and endothelial dysfunction, promoting atrial remodeling and fibrillation persistence. Moreover, glycemic variability has been implicated in arrhythmogenesis and myocardial fibrosis through modulation of reactive oxygen species and impaired signaling pathways.
Clinically, serial monitoring of the TyG index—reflecting integrated metabolic stress and IR—could enable early identification of high-risk AF patients warranting closer surveillance and tailored therapeutic strategies. Considering that TyG components are routinely measured in ICU labs, implementing trajectory analyses is feasible and cost-effective.
Nonetheless, there are limitations: the observational retrospective design precludes causal inference; the single-center US cohort may limit external generalizability; and non-fasting samples may introduce variability in TyG calculation. Future prospective multicenter studies are warranted to validate these findings and to explore whether targeted interventions on metabolic parameters can improve outcomes in this vulnerable population.
Conclusion
In critically ill patients with atrial fibrillation admitted to ICUs, distinct trajectories of the triglyceride-glucose index, particularly high-level fluctuations during ICU stay, are independently associated with increased short- and long-term all-cause mortality. These results support the TyG index trajectory as a novel and practical biomarker for risk stratification and prognosis in this high-risk group. Integration of dynamic metabolic monitoring into ICU care protocols may enhance patient management and improve survival outcomes.