Highlights
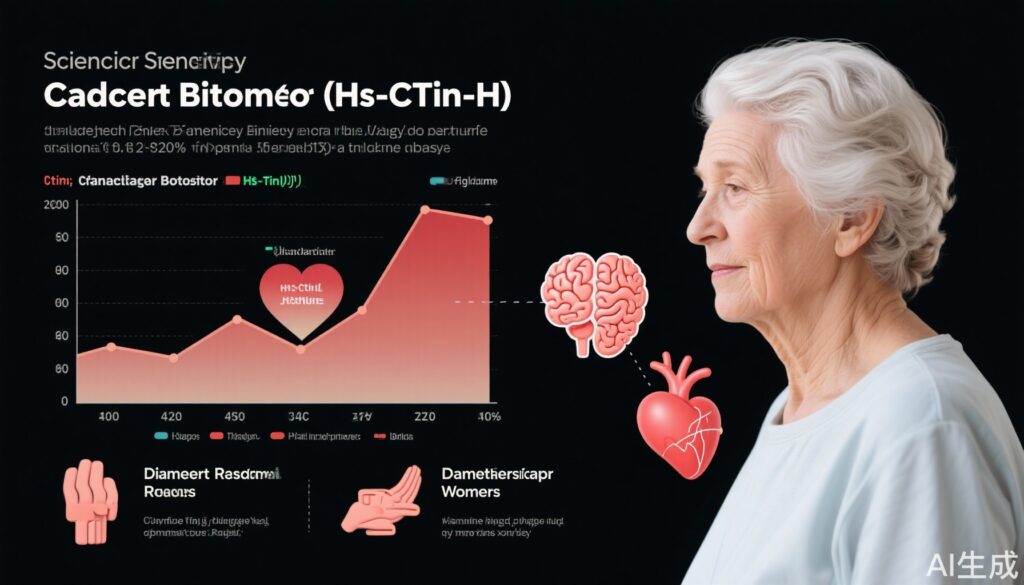
- Subclinical elevations of high-sensitivity cardiac troponin I (hs-cTnI), even below the 99th percentile for myocardial injury, predict increased risk of late-life dementia (LLD) in older women.
- In a 14.5-year longitudinal cohort study, higher quartiles of hs-cTnI correlated with higher incidence of LLD events, hospitalisations, and dementia-related deaths, independent of APOE genotype and established risk factors.
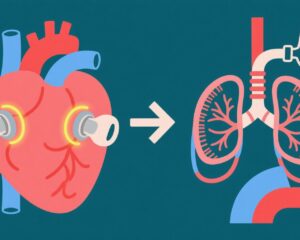
- Hs-cTnI may serve as a valuable biomarker integrating cardiovascular and neurodegenerative disease risk, supporting the interconnected pathophysiology between cardiac and brain health vulnerabilities in ageing.
Background
Late-life dementia (LLD) is a major public health challenge characterized by progressive cognitive decline, imposing significant societal and economic burdens globally. Cardiovascular disease (CVD) and cognitive impairment share overlapping risk profiles, with mounting evidence linking myocardial injury markers to dementia pathogenesis. High-sensitivity cardiac troponin I (hs-cTnI), a sensitive biomarker of myocardial injury, has been established as a predictor of cardiovascular outcomes. However, the prognostic significance of subclinical hs-cTnI elevations below the sex-specific 99th percentile threshold for myocardial injury, especially in relation to LLD, remains less well-understood, particularly in elderly women, a population disproportionately affected by dementia. The Perth Longitudinal Study of Ageing Women provides a unique opportunity to investigate this association over an extended follow-up period.
Key Content
Study Design and Methods
The study prospectively enrolled 986 community-dwelling women aged 70 years or older, free from prior diagnosis of LLD, and with baseline hs-cTnI levels below 15.6 ng/L, the sex-specific 99th percentile cut-off indicating myocardial injury. Participants were stratified into quartiles according to hs-cTnI levels (Q1 median 3.1 ng/L to Q4 median 7.3 ng/L). Incident LLD-related events, defined as hospitalisation due to dementia or death with dementia, were tracked over 14.5 years via linked health records. Extensive multivariable Cox proportional hazards models adjusted for comprehensive cardiovascular and dementia risk factors—including APOE genotype—analyzed associations.
Principal Findings
At baseline, the mean age was 75.2 ± 2.7 years. Over the follow-up, 174 LLD events (17.7%), 155 hospitalisations (15.7%), and 68 deaths (6.9%) due to dementia were recorded. Compared with the lowest quartile (Q1), women in the highest quartile (Q4) demonstrated significantly increased risks:
- LLD-related events: Adjusted hazard ratio (HR) 1.88 (95% CI: 1.22–2.91)
- Hospitalisations: Adjusted HR 1.65 (95% CI: 1.04–2.64)
- Dementia-related death: Adjusted HR 2.27 (95% CI: 1.13–4.59)
These associations persisted after controlling for conventional dementia and cardiovascular risk factors, including genetics (APOE genotype).
Integration with Current Understanding and Related Evidence
This study complements growing literature implicating subclinical myocardial injury, vascular dysfunction, and chronic neuroinflammation as common pathways in the pathogenesis of dementia. Neurodegenerative mechanisms—such as mitochondrial dysfunction, oxidative stress, and neuroinflammation—intersect with cardiovascular pathology, as described in recent reviews emphasizing pathways linking cardiovascular biomarkers and neurodegeneration. Moreover, APOE genotype remains a pivotal genetic modulator of dementia risk and neuroinflammatory responses; its inclusion in the adjustment enhances confidence that hs-cTnI is an independent predictive marker.
Emerging therapeutic strategies targeting vascular health, inflammation modulation, and mitochondrial protection hold potential in altering dementia trajectories. These findings underscore the need for integrated biomarker approaches to identify at-risk individuals early, potentially enabling preventive interventions.
Expert Commentary
The current evidence underscores the utility of hs-cTnI beyond traditional cardiovascular prognostication, proposing a role in dementia risk stratification. The biological plausibility relates to shared vascular injury and neurodegenerative pathways contributing to cognitive decline in ageing. However, the determination of causality remains complex given the multifactorial nature of LLD. As hs-cTnI assays become standardized and widely accessible, their incorporation into multifactorial risk models may refine individual risk assessment.
Clinically, these findings prompt vigilance in managing cardiovascular health as part of dementia prevention, especially in older women, who face disproportionately higher LLD risk. Future research should elucidate whether interventions modulating subclinical myocardial injury can delay or prevent dementia onset. Additionally, the potential of hs-cTnI as a monitoring biomarker for therapeutic efficacy in multidomain prevention trials warrants exploration.
Limitations include observational design restrictions, potential unmeasured confounding, and generalizability limited to elderly women of similar demographics. Moreover, the mechanisms mediating the observed associations require further mechanistic and translational studies.
Conclusion
Hs-cTnI levels below the 99th percentile for myocardial injury are independently associated with increased risks of late-life dementia events, hospitalization, and death in older women over 14.5 years. This novel finding supports the hypothesis that subclinical cardiac injury biomarkers reflect an integrated cardiovascular-brain vulnerability underlying dementia risk. Incorporating hs-cTnI measurement may enhance early identification of women at elevated risk, enabling targeted preventive strategies. Further prospective studies and mechanistic research are essential to validate findings and guide clinical integration.
References
- Toro-Huamanchumo CJ et al. Association of high-sensitivity cardiac troponin I levels below the sex-specific 99th percentile with late-life dementia: the Perth Longitudinal Study of Ageing Women. Heart. 2025 Aug 19:heartjnl-2025-326066. doi:10.1136/heartjnl-2025-326066. PMID: 40830043.
- Additional recent reviews on neurodegenerative mechanisms, cardiovascular biomarkers, and APOE genotype implications cited from Neural Regen Res (2026), providing mechanistic context.