Introduction
Type 2 diabetes (T2D) presents a significant health burden, particularly among United States veterans who face a disproportionately high prevalence and complexity of comorbid conditions. Veteran populations often contend with compounded challenges such as psychosocial stressors, multimorbidity, and barriers to healthcare access, which can hinder effective diabetes management. Traditional treatment regimens relying heavily on medication intensification frequently encounter issues related to adherence and patient preferences. Hence, innovative, accessible interventions that provide continuous support and empower veterans to manage T2D effectively are critically needed.
Remote telemedicine interventions offer promise for overcoming geographic and logistical barriers in this population. However, many telemedicine programs lack sustained engagement and comprehensive support, limiting long-term clinical impact. A ketogenic nutrition program delivered via continuous remote care—integrating individualized coaching, real-time biomarker monitoring, and medication management—may offer an effective, scalable approach to improve metabolic outcomes in veterans with T2D.
This article critically evaluates findings from a 3-year retrospective observational study examining the long-term effectiveness and safety of a remotely delivered ketogenic nutrition therapy program designed and delivered by Virta Health in collaboration with the Veterans Health Administration (VHA).
Study Design and Population
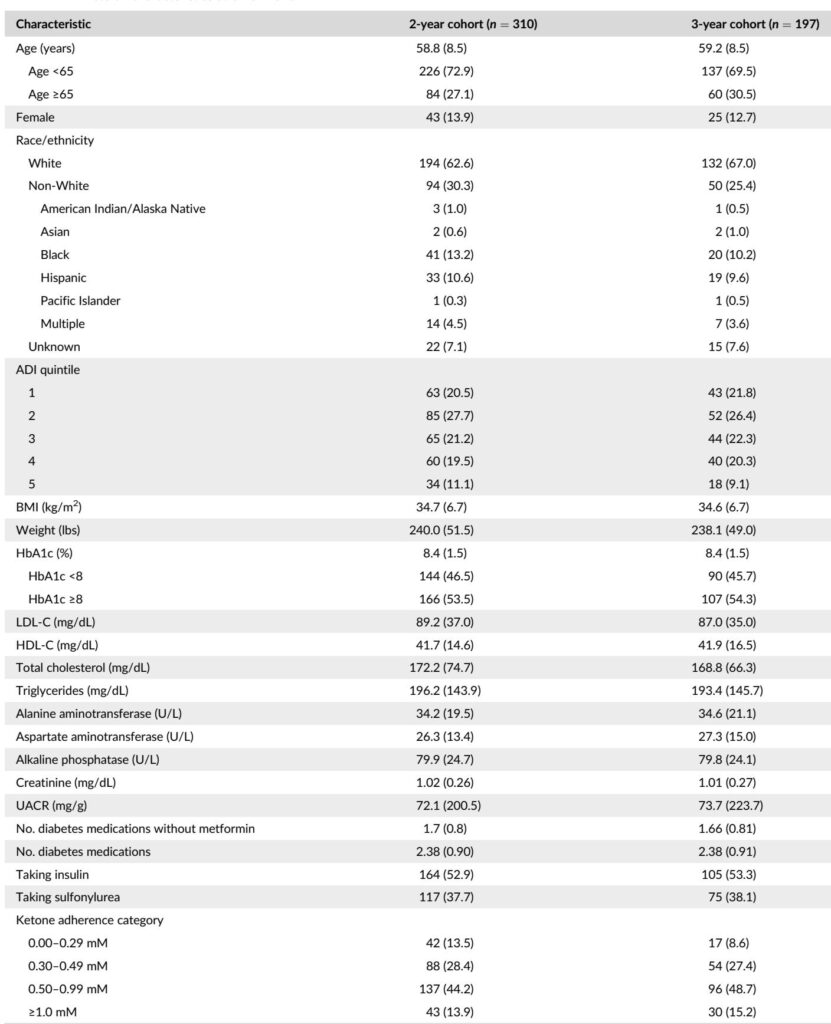
This retrospective observational analysis included 640 veterans diagnosed with T2D who enrolled in a continuous remote care intervention featuring a medically supervised ketogenic diet. Eligibility criteria required VHA enrollment, confirmed T2D diagnosis (HbA1c ≥6.5%), and use of at least one diabetes medication besides metformin. Veterans with advanced organ dysfunction or severe comorbidities were excluded.
The intervention was fully telemedicine-based and delivered via a mobile app, enabling veterans to receive sustained coaching from medical providers and health coaches, monitor blood glucose and ketone levels using connected devices, and receive personalized adjustments to their nutrition plan and medication regimen. The ketogenic diet prescribed was low in carbohydrates, high in fat, and moderate in protein to induce nutritional ketosis.
Participants were followed up to three years, with primary endpoints consisting of changes in hemoglobin A1c (HbA1c) and body weight at 2 and 3 years. Secondary outcomes included diabetes medication use and cardiometabolic markers such as lipid profiles, liver enzymes, and kidney function indices. Subgroup analyses examined differential outcomes by age, race/ethnicity, socioeconomic disadvantage (Area Deprivation Index), baseline glycemic control, medication status, and early ketone adherence.
Key Findings
Of the 640 enrolled veterans, 49% (n=310) remained engaged at 2 years, and 33% (n=197) at 3 years. Baseline characteristics reflected a mean age of 59 years, mean BMI of 35 kg/m², and mean HbA1c of 8.4%. Veterans who remained enrolled tended to be slightly older, had lower baseline HbA1c, and demonstrated higher early ketone adherence.
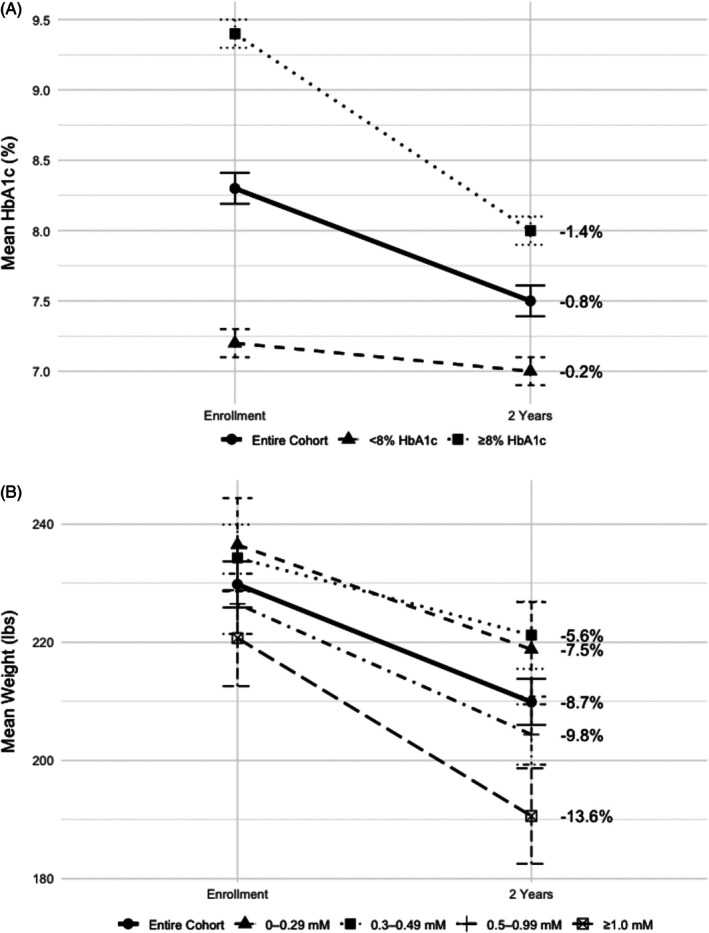
At both 2 and 3 years, veterans who remained active in the program showed sustained metabolic improvements:
– HbA1c decreased by approximately 0.8%, from an average of 8.3–8.4% to 7.4–7.5%, reflecting clinically meaningful glycemic control enhancements known to reduce risks of microvascular and macrovascular complications.
– Body weight decreased by roughly 9%, corresponding to an average weight loss of 19.9 pounds at 2 years and 21.8 pounds at 3 years.
– Diabetes medication utilization declined substantially, including a 17–19% reduction in insulin use and marked decreases in sulfonylureas and DPP-4 inhibitors. Among insulin users, average daily dose reduced by 61–68%.
– Cardiometabolic markers, including HDL cholesterol and liver enzymes (alanine and aspartate aminotransferase), showed favorable shifts, while total cholesterol, LDL cholesterol, triglycerides, and kidney function markers remained stable, indicating a generally safe metabolic profile.
Veterans who discontinued participation before 2 years nevertheless experienced meaningful metabolic improvements at departure, especially if enrolled for ≥6 months. Weight loss averaged 6% for those enrolled longer than 6 months, accompanied by reductions in glucose levels and diabetes medication use.
Subgroup analyses revealed that HbA1c improvements were most pronounced in veterans with baseline HbA1c ≥8%, with reductions averaging 1.3%. In contrast, those with baseline HbA1c <8% maintained stable glycemic control with reduced medication reliance. Weight loss was consistent across race, age, socioeconomic status, and diabetes medication status, though white veterans and those on insulin at baseline experienced slightly greater weight reductions. Higher early ketone adherence correlated with increased weight loss, underscoring the importance of early dietary compliance.
Expert Commentary
This study substantiates previous clinical trial findings on the efficacy of ketogenic diets for diabetes management and expands them within a real-world veteran population over an extended follow-up period. The integration of continuous remote monitoring and individualized support appears instrumental in sustaining dietary adherence and optimizing clinical outcomes.
The observed HbA1c reductions of approximately 0.8–1.3% and 9% weight loss are comparable with leading pharmacologic agents such as GLP-1 receptor agonists and signify substantial clinical benefit. Importantly, these improvements were achieved alongside substantial medication de-escalation, highlighting the potential for carbohydrate restriction to reduce therapy burden.
Limitations include the observational design and attrition over time, which may bias results toward more engaged and responsive veterans. While the study lacked a randomized control group, complementary quasi-experimental analyses by Strombotne et al. support the intervention’s cost-effectiveness and clinical benefits.
The safety profile was reassuring with stable kidney and lipid parameters, though longer prospective studies are warranted to evaluate cardiovascular and renal event outcomes definitively. Addressing slight disparities in weight loss by race could enhance equitable implementation.
Conclusion
This 3-year observational study demonstrates that a remotely delivered, continuous care ketogenic nutrition program can produce durable, clinically significant metabolic improvements in veterans with type 2 diabetes. Sustained participation yields meaningful reductions in HbA1c and weight, decreases reliance on diabetes medications, and maintains safety markers. Shorter participation also confers notable benefits.
The findings underscore the value of integrating evidence-based ketogenic dietary interventions within veteran healthcare systems, facilitated by telemedicine, to overcome traditional care barriers and enhance diabetes management. Future research should focus on long-term cardiovascular outcomes, reasons for discontinuation, and strategies to optimize adherence and equitable results.
This intervention represents a promising addition to the repertoire of diabetes management options for veterans, offering a personalized, patient-centered approach aligned with preferences for medication minimization and sustained metabolic health.
Reference
Adams RN, Athinarayanan SJ, Zoller AR, McKenzie AL, Ratner RE. Sustained metabolic improvements in a remotely delivered ketogenic nutrition programme for veterans with type 2 diabetes: A 3-year observational study. Diabetes Obes Metab. 2025 Sep;27(9):4825-4835. doi: 10.1111/dom.16525 IF: 5.7 Q1 . Epub 2025 Jun 16. PMID: 40521806 IF: 5.7 Q1 ; PMCID: PMC12326886 IF: 5.7 Q1 .