Highlight
– The Cutaneous Lymphoma International Consortium analyzed survival in 1,275 patients with advanced mycosis fungoides (MF) and Sézary syndrome (SS).
– Four independent prognostic markers—stage IV disease, age over 60, large-cell transformation, and elevated lactate dehydrogenase (LDH)—were linked to worse survival.
– A prognostic index categorizing patients into low, intermediate, and high risk groups demonstrated distinct 5-year survival rates of 68%, 44%, and 28%, respectively.
– This large multicenter dataset provides a new tool to refine prognosis and guide treatment strategies in advanced MF/SS.
Study Background
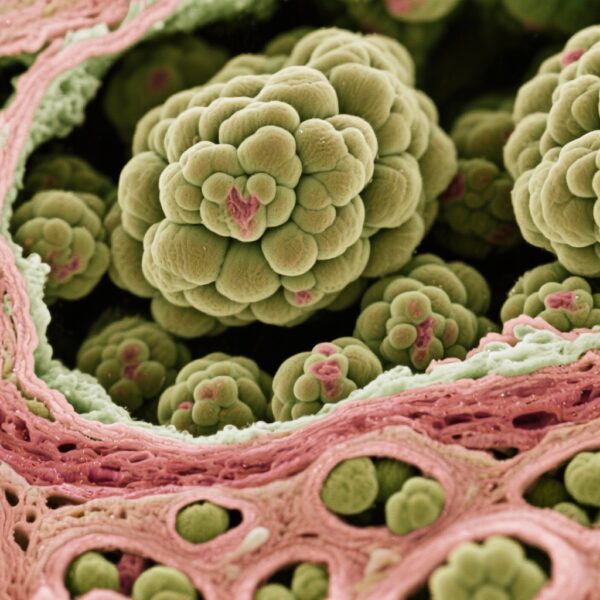
Mycosis fungoides (MF) and Sézary syndrome (SS) are the most common subtypes of cutaneous T-cell lymphoma (CTCL), characterized by malignant proliferation of skin-homing T cells. While early stages of MF may have indolent behavior with excellent prognosis, advanced-stage MF (stage IIB-IV) and SS present aggressive clinical courses with median survival ranging from 1 to 5 years. Treatment approaches are predominantly stage-based; however, outcomes vary considerably within similar stages, reflecting underlying biological and clinical heterogeneity.
Historically, prognostic information has been derived from small, primarily single-center studies, limiting definitive conclusions due to rare disease prevalence. Identification of robust, independent prognostic factors through large-scale international collaboration could enable improved stratification of advanced-stage patients, informing clinical decisions and clinical trial design.
Study Design
This was a retrospective cohort study conducted under the Cutaneous Lymphoma International Consortium, assembling clinical data from 29 international specialist centers. The study population comprised 1,275 patients diagnosed with advanced-stage MF or SS (stage IIB to IV) from 2007 onwards.
A comprehensive literature review identified ten candidate prognostic variables to test for independent associations with overall survival (OS). These included clinical parameters (disease stage, age, sex), histopathologic features (folliculotropism, CD30 positivity, large-cell transformation), biological markers (proliferation index, serum lactate dehydrogenase levels), blood counts (white blood cell and lymphocyte counts), and molecular findings (identical T-cell clone presence in blood and skin).
Each parameter was assessed at diagnosis. The primary endpoint was overall survival, calculated from diagnosis to death or last follow-up.
Key Findings
The median overall survival (OS) for the cohort was 63 months. Two- and five-year survival rates were 77% and 52%, respectively.
Stratified by stage:
– Stage IIB patients had a median OS of 68 months.
– Surprisingly, stage III patients exhibited slightly better survival compared to stage IIB.
– Stage IV patients had markedly worse outcomes: median OS was 48 months for IVA and 33 months for IVB.
Of the ten candidate variables, four were identified as independent adverse prognostic factors through multivariate analysis:
– Stage IV disease
– Age greater than 60 years
– Presence of large-cell transformation (histologic shift to large atypical malignant cells)
– Elevated serum lactate dehydrogenase (LDH) levels, reflecting tumor burden or cell turnover
Utilizing these markers, a prognostic index was developed, categorizing patients into three risk groups regardless of clinical stage:
– Low risk (none or one adverse factor): 5-year OS of 68%
– Intermediate risk (two adverse factors): 5-year OS of 44%
– High risk (three or four adverse factors): 5-year OS of 28%
This model refined prognostic stratification beyond traditional staging alone.
Expert Commentary
The study represents the largest international dataset assessing advanced MF and SS prognosis, addressing prior limitations of small cohorts. By systematically evaluating multiple clinicopathologic and molecular factors, the authors have elucidated key determinants of survival that can inform patient counseling and clinical trial stratification.
The finding that stage III patients fared unexpectedly better than stage IIB may reflect heterogeneity in skin versus nodal involvement or sampling biases. Large-cell transformation emerged as a robust marker of aggressive biology, consistent with prior literature.
Elevated LDH is a nonspecific but valuable indicator of tumor activity and is readily available in clinical practice. Age remains a critical risk modifier, likely reflecting comorbidities and tolerance to therapies.
Limitations include retrospective design, potential inter-center variability in clinical assessments, and missing data for some markers such as proliferation index and CD30 expression, which did not emerge as independent factors here but merit further investigation.
Future prospective studies integrating genomic and immunologic profiling may enhance the prognostic precision.
Conclusion
This collaborative international study significantly advances the understanding of prognostic factors in advanced-stage MF and SS. By integrating disease stage, age, histopathologic transformation, and laboratory markers into a prognostic index, clinicians can better stratify patients by risk, enabling more personalized therapeutic approaches and optimizing enrollment for clinical trials.
As the therapeutic landscape evolves with novel agents, robust risk stratification will be essential to improve outcomes in these challenging cutaneous lymphomas.
Funding and Registration
The study was supported by the Cutaneous Lymphoma International Consortium with contributions from participating academic centers. No specific clinicaltrials.gov registration was reported.
References
Scarisbrick JJ, Prince HM, Vermeer MH, et al. Cutaneous Lymphoma International Consortium Study of Outcome in Advanced Stages of Mycosis Fungoides and Sézary Syndrome: Effect of Specific Prognostic Markers on Survival and Development of a Prognostic Model. J Clin Oncol. 2015 Nov 10;33(32):3766-73. doi:10.1200/JCO.2015.61.7142. PMID: 26438120; PMCID: PMC4979132.