Highlight
- Distinct gut microbial profiles correlate with specific ADHD core symptoms, with combined presentations showing greatest alterations.
- Beneficial bacteria involved in short-chain fatty acid (SCFA) synthesis, especially Lactobacillus sanfranciscensis, are significantly reduced in ADHD patients.
- Imidazoleacetic acid mediates the link between Lactobacillus sanfranciscensis abundance and inattention, suggesting a metabolic pathway connecting microbiota changes to ADHD symptoms.
- Fecal microbiota transplantation in mice validates that restoring Lactobacillus sanfranciscensis ameliorates hyperactivity and inattention, while acetate supplementation specifically improves attention deficits.
Study Background and Disease Burden
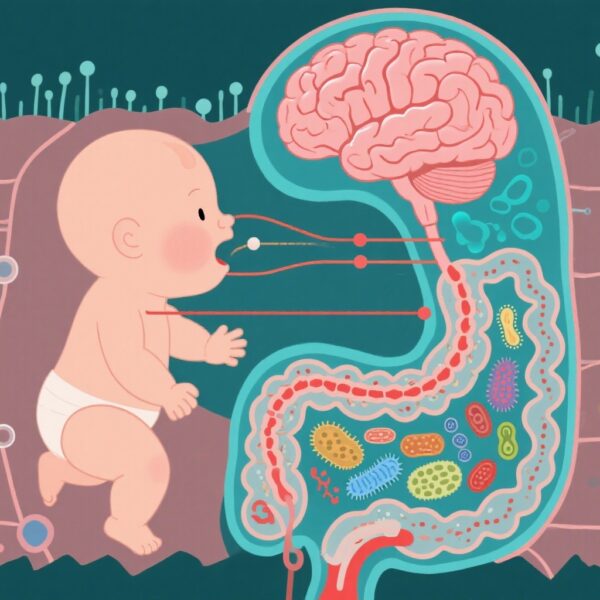
Attention-deficit/hyperactivity disorder (ADHD) is a prevalent neurodevelopmental condition characterized by inattention, hyperactivity, and impulsivity. It affects children and adults worldwide, imposing substantial psychosocial and economic burdens. Despite extensive research, the precise biological mechanisms remain incompletely understood, limiting therapeutic strategies. Emerging evidence implicates the gut-brain axis, an interactive system linking gut microbiota to central nervous system function, as a contributor to neurodevelopmental disorders including ADHD. However, studies have not definitively identified the gut microbial species or metabolites that correspond to specific ADHD symptoms or revealed the mechanistic pathways underlying these associations. Understanding symptom-specific microbial and metabolic alterations could open novel avenues for targeted interventions.
Study Design
This investigation employed a case-control design involving 94 ADHD patients and 94 age- and gender-matched healthy controls. Comprehensive shotgun metagenomic sequencing of fecal samples characterized microbial taxa and functional pathways. Concurrent fecal metabolomics profiling enabled assessment of metabolic alterations related to gut microbiota changes. ADHD patients were stratified into three subgroups based on their core symptom presentations — inattentive, hyperactive-impulsive, and combined types — allowing symptom-specific analyses. A metabolic model was constructed to identify metabolites mediating the relationship between microbiota alterations and behavioral symptoms using causal mediation analysis. To validate clinical findings, fecal microbiota transplantation (FMT) experiments were conducted in mice, assessing behavioral outcomes following administration of feces from patients with low abundance of Lactobacillus sanfranciscensis. The effect of supplementation with this specific bacterial strain and acetate on ADHD-relevant behaviors was also evaluated.
Key Findings
Beta diversity analysis demonstrated that ADHD core symptoms influenced gut microbial community composition significantly (F = 1.345, pFDR = 0.015). Combined presentation (ADHD-C) patients exhibited the most pronounced microbial alterations compared to controls and other subgroups. Several beneficial taxa, particularly those involved in the synthesis of short-chain fatty acids (SCFAs), were significantly downregulated in ADHD groups; among these, Lactobacillus sanfranciscensis showed strong negative correlations with inattention, hyperactivity, and impulsivity (adjusted p-values ranging from 1.04E-13 to 2.61E-05).
Functionally, pathway analysis revealed disruptions in metabolic routes linked to SCFA production and amino acid metabolism. Metabolomic profiling identified multiple metabolites differing across ADHD symptom domains, with imidazoleacetic acid emerging as a partial mediator between Lactobacillus sanfranciscensis abundance and attentional deficits (p = 0.012). This finding suggests that microbial shifts may exert behavioral effects via specific metabolic intermediates.
In vivo validation through fecal microbiota transplantation in mice confirmed the pathogenic role of microbiota composition. Mice receiving feces from ADHD patients with low Lactobacillus sanfranciscensis exhibited increased hyperactivity and attention deficits. Supplementation with this bacterial strain significantly improved both hyperactivity (t = 2.665, p = 0.0237) and inattention (t = 2.389, p = 0.0380), whereas acetate supplementation selectively ameliorated inattention (t = 2.362, p = 0.0398). These results underscore SCFA deficiency, particularly acetate, as a key pathogenic mechanism and highlight Lactobacillus sanfranciscensis as a therapeutic candidate.
Expert Commentary
This sophisticated study is among the first to disentangle symptom-specific gut microbial profiles in ADHD and to elucidate mechanistic links via metabolic mediation. The use of shotgun metagenomics combined with metabolomics and causal mediation analyses provides robust multi-omics insight surpassing previous correlational reports. Importantly, the translation of human findings into an animal model with fecal microbiota transplantation allows for causal inference and intervention testing.
By identifying SCFA-producing Lactobacillus species as protective taxa and demonstrating partial rescue of symptoms with bacterial and acetate supplementation, the study provides compelling evidence that SCFA deficiency contributes to ADHD pathogenesis. These findings align with growing literature supporting the gut microbiome as a modifiable factor in neurodevelopmental disorders. The partial mediation by imidazoleacetic acid further suggests complex metabolic interplay, inviting deeper exploration.
However, limitations include the observational nature of most human data, potential confounding factors such as diet or medication usage, and the challenge of translating murine behavioral assays fully to human ADHD features. Longitudinal studies and clinical trials of microbiota-targeted therapies are needed to confirm therapeutic value and causality.
Conclusion
This comprehensive study advances our understanding of ADHD by demonstrating that gut microbial composition varies with symptom profiles and that short-chain fatty acid deficiency, driven by reduced Lactobacillus sanfranciscensis, underlies key pathogenic mechanisms. Metabolic alterations, including changes in imidazoleacetic acid, appear to mediate microbiota-behavior interactions. Animal model validations support a causal role and the potential for microbiota-based interventions.
The integration of symptom-specific microbial and metabolic profiling heralds a precision medicine approach for ADHD, where targeted restoration of SCFA-producing bacteria could complement existing treatments. Future research should explore clinical trials of probiotic supplementation and elucidate detailed metabolomic pathways to optimize therapeutic strategies.
References
Wang X, Wang N, Gao T, Zhang Y, Fu Z, Zhao Y, Huang Y, Zheng X, Gao X, Lu L, Yang L. Symptom-specific gut microbial and metabolic profiles in ADHD reveal SCFA deficiency as a Key pathogenic mechanism. Gut Microbes. 2025 Dec;17(1):2537755. doi: 10.1080/19490976.2025.2537755. Epub 2025 Jul 27. PMID: 40719366; PMCID: PMC12309550.
Jiang HY, Ling ZX, Zhang YH, Mao HJ, Ma ZP, Yin Y, Wang W, Tang W, Tan Z, Shi J, Li L, Ruan B. Altered gut microbiota profile in patients with generalized anxiety disorder. J Psychiatr Res. 2018 May;104:130-136. doi: 10.1016/j.jpsychires.2018.07.007.
Hsiao EY, McBride SW, Hsien S, Sharon G, Hyde ER, McCue T, Codelli JA, Chow J, Reisman SE, Petrosino JF, Patterson PH, Mazmanian SK. Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell. 2013 Dec 19;155(7):1451-1463. doi: 10.1016/j.cell.2013.11.024.
Sarkar A, Lehto SM, Harty S, Dinan TG, Cryan JF, Burnet PW. Psychobiotics and the Manipulation of Bacteria–Gut–Brain Signals. Trends Neurosci. 2016 Nov;39(11):763-781. doi: 10.1016/j.tins.2016.07.002.