Study Background and Disease Burden
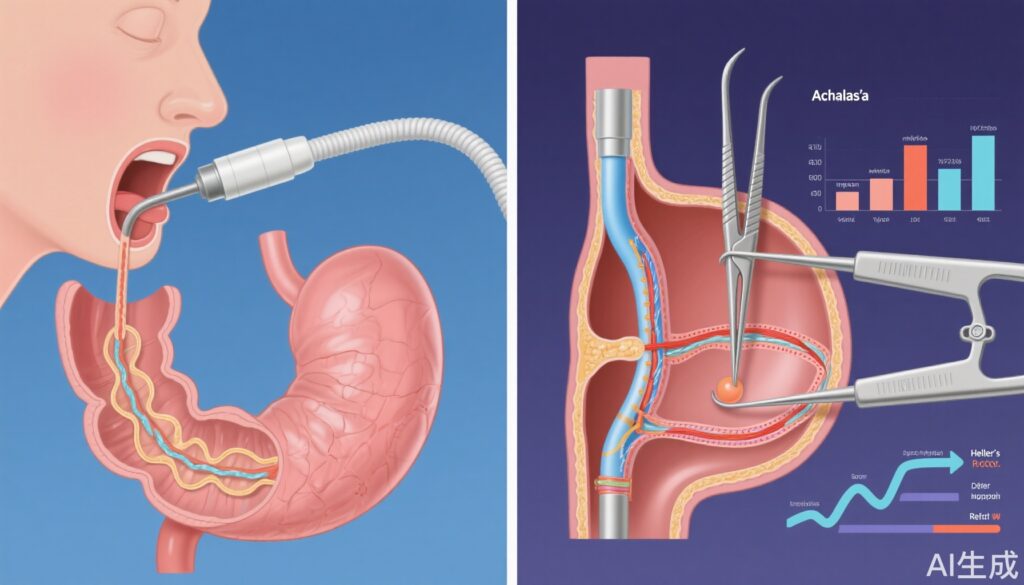
Idiopathic achalasia is a rare esophageal motility disorder characterized by impaired relaxation of the lower esophageal sphincter (LES) and absent peristalsis, leading to symptoms such as dysphagia, regurgitation, and chest pain. It significantly impairs quality of life and may lead to complications including esophageal dilation and increased risk for esophageal cancer. The current standard treatments involve disrupting the LES muscle to relieve obstruction, traditionally by surgical methods like laparoscopic Heller’s myotomy (LHM) combined with Dor fundoplication to prevent reflux. Recently, per-oral endoscopic myotomy (POEM), a less invasive endoscopic technique, has emerged as an alternative. While initial results up to 2 years post-treatment demonstrated similar effectiveness between POEM and LHM plus Dor fundoplication, concerns remained regarding gastro-esophageal reflux disease (GERD) incidence, with increased reflux events after POEM. This necessitated a longer-term comparative assessment to guide clinical decision-making.
Study Design
This multicentre, randomized, open-label, non-inferiority trial enrolled patients with symptomatic primary achalasia from eight centers across six European countries between 2012 and 2015. Eligible adults (aged >18 years) had an Eckardt symptom score greater than 3, indicating active disease. Participants were randomized in a 1:1 ratio to receive either POEM or LHM plus Dor fundoplication. The primary endpoint, previously reported at 2 years, assessed clinical success defined as an Eckardt score ≤3 without additional treatment. Secondary endpoints collected at 5 years included clinical success, Eckardt scores, Gastrointestinal Quality of Life Index (GIQLI) scores, LES function measured by high-resolution manometry, and reflux parameters assessed by endoscopy (Los Angeles classification), pH-metry, and the DeMeester clinical score. The study utilized a modified intention-to-treat (mITT) approach including all patients who received their assigned procedure. The non-inferiority margin was set at -12.5 percentage points for the difference in clinical success rates.
Key Findings
A total of 241 patients were randomized, with 221 receiving assigned treatments (112 POEM, 109 LHM). At 5 years, follow-up data were available for 177 patients (90 POEM, 87 LHM). Clinical success rates were 75.0% (95% CI, 66.2–82.1) for POEM and 70.8% (61.7–78.5) for LHM plus Dor fundoplication (difference +4.2 percentage points, 95% CI -7.4 to 15.7), confirming POEM’s non-inferiority with sustained symptom control.
Both groups experienced significant reductions in mean Eckardt symptom scores from baseline to 5 years, with a non-significant difference favoring POEM (mean difference -0.29; 95% CI -0.62 to 0.05). GIQLI scores and LES integrated relaxation pressure measurements similarly showed no significant differences between groups over time.
Regarding reflux, endoscopic evidence of reflux esophagitis was more frequent after POEM (41% of 63 patients) versus LHM (31% of 58 patients), though the difference was not statistically conclusive (10.2 percentage points, 95% CI -7.0 to 26.8). Notably, more patients in the POEM group exhibited significant esophagitis (Los Angeles grade B, C, or D: 14% vs 7%). pH-metry, conducted in 37% of participants, revealed that POEM patients had higher mean acid exposure times (10.2%) compared to those receiving LHM (5.5%). The proportion with abnormal acid exposure (>4.5%) was significantly greater in the POEM group (62%) than in the LHM group (31%), indicating a higher reflux burden after POEM.
Despite differences in objective reflux measures, patient-reported reflux symptoms at 5 years were similar between groups, with DeMeester clinical scores averaging 1.3 after POEM and 1.1 after LHM. No major reflux-related complications such as peptic strictures, Barrett’s esophagus, or esophageal adenocarcinoma were reported during this follow-up period.
Expert Commentary
This landmark multicentre trial provides robust long-term evidence supporting POEM as a minimally invasive alternative to the standard LHM plus Dor fundoplication for idiopathic achalasia. The comparable clinical success rates underscore POEM’s efficacy in symptom control up to 5 years, expanding the therapeutic armamentarium. However, consistent with earlier findings, POEM carries a higher risk of reflux esophagitis and abnormal acid exposure compared to LHM with fundoplication, likely due to the lack of an anti-reflux surgical wrap.
These findings highlight the importance of careful patient selection and counseling. Clinicians must balance the benefits of a less invasive procedure against potentially increased reflux risk and tailor surveillance accordingly. While the absence of significant reflux-related complications is reassuring, longer-term data are needed to assess cumulative risks of Barrett’s esophagus and neoplasia. The open-label design and variable pH-metry uptake are limitations but reflect pragmatic, real-world practice.
Conclusion
In conclusion, POEM is a clinically effective, less invasive option for idiopathic achalasia with sustained symptom control comparable to laparoscopic Heller’s myotomy plus Dor fundoplication at 5 years. However, a higher incidence of gastroesophageal reflux disease following POEM warrants vigilant post-procedural monitoring and patient education regarding potential reflux symptoms and complications. Future research should focus on optimizing reflux prevention strategies after POEM and longer-term surveillance protocols.
References
Hugova K, Mares J, Hakanson B, Repici A, von Rahden BHA, Bredenoord AJ, Bisschops R, Messmann H, Ruppenthal T, Mann O, Izbicki J, Harustiak T, Fumagalli Romario U, Rosati R, Germer CT, Schijven M, Emmermann A, von Renteln D, Dautel S, Fockens P, Boeckxstaens G, Rösch T, Martinek J, Werner YB. Per-oral endoscopic myotomy versus laparoscopic Heller’s myotomy plus Dor fundoplication in patients with idiopathic achalasia: 5-year follow-up of a multicentre, randomised, open-label, non-inferiority trial. Lancet Gastroenterol Hepatol. 2025 May;10(5):431-441. doi: 10.1016/S2468-1253(25)00012-3. PMID: 40112837.