Highlight
Postoperative pancreatic fistula (POPF) is a significant complication following pancreaticoduodenectomy. This comprehensive Cochrane review update synthesizes randomized controlled trial (RCT) evidence comparing duct-to-mucosa pancreaticojejunostomy with other anastomotic techniques, including invagination and binding methods, to determine the best reconstructive approach to minimize POPF.
The analysis includes 14 RCTs with 2140 adults undergoing open pancreaticoduodenectomy and finds very low-certainty evidence that duct-to-mucosa technique may not reduce POPF incidence, postoperative mortality, or other complications compared to other techniques.
No definitive superiority between different duct-to-mucosa pancreaticojejunostomy methods (modified Blumgart vs. traditional interrupted sutures) was observed, underscoring uncertainty and the importance of surgeon preference and expertise.
Study Background
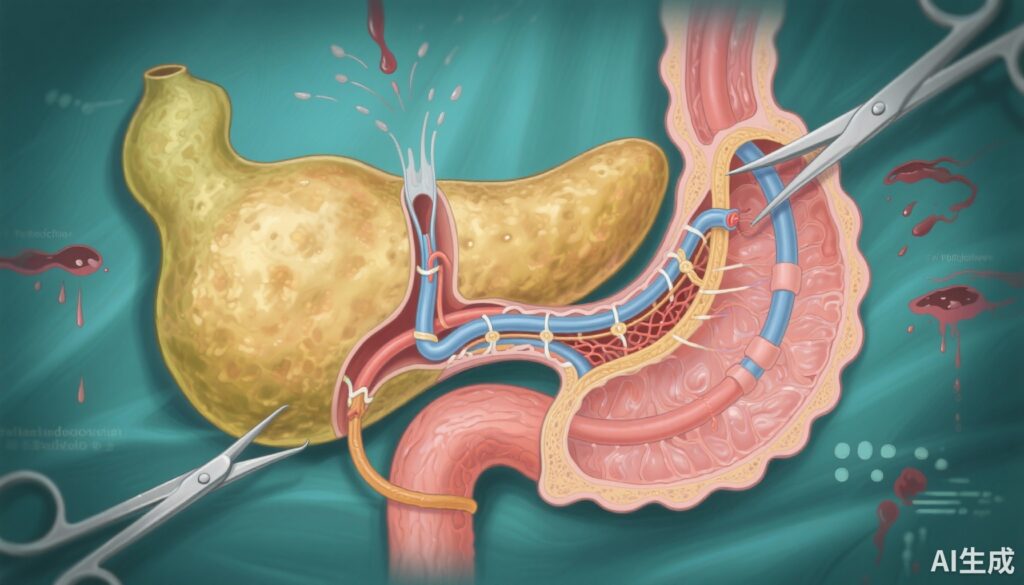
Pancreaticoduodenectomy, or Whipple procedure, is a complex surgery often performed for pancreatic head tumors and periampullary diseases. Reconstruction involves creating an anastomosis between the pancreatic remnant and the jejunum to restore digestive continuity. However, the procedure carries a high risk of postoperative pancreatic fistula (POPF), a complication where leakage of pancreatic fluid leads to morbidity, prolonged hospitalization, and mortality.
Various pancreaticojejunostomy techniques—including duct-to-mucosa and invagination anastomoses—have been developed with the goal of reducing POPF rates. The duct-to-mucosa technique involves precise suturing of the pancreatic duct to the jejunal mucosa, theoretically offering better drainage. Despite its common use, clarity on its superiority over other methods remains lacking due to conflicting data and methodological limitations.
Study Design
This systematic review and meta-analysis updated a 2022 Cochrane review, incorporating three new randomized controlled trials up to June 2024. Eligible studies included adults (≥18 years) undergoing open pancreaticoduodenectomy comparing duct-to-mucosa pancreaticojejunostomy against other techniques such as invagination and binding methods. Studies comparing different duct-to-mucosa approaches (modified Blumgart versus traditional interrupted technique) were also included.
Primary outcomes were grade B or C POPF rate, postoperative mortality, and adverse events, while secondary outcomes included surgical re-interventions, postoperative bleeding, overall surgical complications, and length of hospital stay. The Cochrane Risk of Bias tool (RoB 1) assessed study quality. Data synthesis used random-effects meta-analysis, with the GRADE approach determining the certainty of evidence.
Key Findings
Fourteen RCTs involving 2140 participants were included; 12 RCTs (1678 patients) compared duct-to-mucosa vs. invagination pancreaticojejunostomy, and two RCTs (462 patients) compared modified Blumgart vs. traditional interrupted duct-to-mucosa techniques. All studies were assessed to have a high risk of bias due to methodological limitations and reporting issues.
Duct-to-mucosa versus other pancreaticojejunostomy techniques: Evidence was very uncertain regarding the benefits of duct-to-mucosa pancreaticojejunostomy. The pooled risk ratio (RR) for POPF was 1.24 (95% CI 0.72 to 2.14), indicating no clear reduction in fistula risk compared to invagination technique. There were also no statistically significant differences in postoperative mortality (RR 1.05, 95% CI 0.59 to 1.86), surgical re-intervention rates (RR 1.43, 95% CI 0.87 to 2.33), postoperative bleeding (RR 1.06, 95% CI 0.69 to 1.63), overall surgical complications (RR 1.10, 95% CI 0.95 to 1.26), or hospital stay duration (mean difference -0.41 days, 95% CI -1.87 to 1.04).
No adverse events were systematically reported.
Duct-to-mucosa modified Blumgart vs. traditional interrupted technique: Limited data from two RCTs suggested no clear benefit or harm of the modified Blumgart technique over the traditional interrupted sutures for any outcome. POPF rate RR was 1.19 (95% CI 0.68 to 2.08), postoperative mortality RR 2.77 (95% CI 0.55 to 13.98), with similarly wide confidence intervals and very low certainty evidence.
The length of hospital stay was non-significantly shorter by an average of 2.62 days (95% CI -6.76 to 1.52) with the modified Blumgart technique, but this result was imprecise.
Expert Commentary
The present comprehensive review highlights persistent uncertainty around reconstructive techniques to prevent POPF—a dreaded and complex postoperative complication. Despite duct-to-mucosa pancreaticojejunostomy being widely adopted due to theoretical advantages of precise pancreatic duct alignment with jejunal mucosa, current evidence does not confirm its superiority over invagination or other techniques.
High risk of bias, heterogeneity in surgical expertise, variable definitions of POPF, and limited adverse events reporting constrain the interpretability and generalizability of findings. Moreover, the subtleties of pancreatic texture, duct size, and intraoperative factors, which influence anastomotic outcomes, remain largely unaccounted for in the aggregate data.
Clinical guidelines and experts often advocate tailoring reconstruction techniques to individual patient and surgeon factors, emphasizing that mastery and experience in a chosen method may be as critical as the method itself. This perspective is supported by the lack of convincing evidence favoring any particular duct-to-mucosa technique variant, such as the modified Blumgart method.
Future well-designed, adequately powered RCTs with standardized outcome assessments, surgical quality control, and thorough adverse event monitoring are sorely needed to resolve these uncertainties and optimize perioperative care.
Conclusion and Clinical Implications
This updated Cochrane review indicates that duct-to-mucosa pancreaticojejunostomy may offer no clear benefit over other pancreatic anastomosis methods in reducing postoperative pancreatic fistula or other complications after pancreaticoduodenectomy. The evidence quality is very low due to methodological limitations and imprecision.
No definitive conclusions can be drawn about the relative merit of duct-to-mucosa technical variants such as the modified Blumgart versus traditional interrupted techniques.
Surgeons should exercise clinical judgment, relying on their experience and patient-specific factors when selecting pancreaticojejunostomy methods. Importantly, patient counseling should include discussion of the current evidence uncertainty and the importance of surgeon expertise.
The sustained high morbidity of POPF underscores an urgent research imperative to develop more effective, standardized surgical techniques and perioperative interventions.
Funding and Trial Registration
This Cochrane review was funded by the National Natural Science Foundation of China (Grant Nos. 81701950, 82172135), Natural Science Foundation of Chongqing (Grant No. CSTB2025NSCQ-GPX1128), Suitable Technology Promotion Project of Chongqing (Grant No. 2024jstg028), Pinnacle Disciplinary Group Joint Project, and the Kuanren Talents Program of the Second Affiliated Hospital of Chongqing Medical University.
Registration: CRD42020169007. Protocol DOI: 10.1002/14651858.CD013462. Original review DOI: 10.1002/14651858.CD013462.pub2.
References
Wu X, Hu L, Zhou S, Liu Z, Gong J, Deng Y, Cheng Y. Duct-to-mucosa versus other types of pancreaticojejunostomy for the prevention of postoperative pancreatic fistula following pancreaticoduodenectomy. Cochrane Database Syst Rev. 2025 Oct 10;10(10):CD013462. doi: 10.1002/14651858.CD013462.pub3. PMID: 41070739; PMCID: PMC12512226.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Lillemoe K, Salvia R, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161(3):584-91.
Asiyanbola B, Gleisner AL, Herman J, et al. Surgical management of the pancreatic remnant after pancreaticoduodenectomy. J Surg Oncol. 2010;101(3):254-259.
Krishna SG, et al. Optimal technique for pancreaticojejunostomy after pancreaticoduodenectomy: a systematic review and meta-analysis. HPB (Oxford). 2016;18(9):723-33.