Highlight
- Deep learning-derived predicted retinal nerve fiber layer (RNFL) thickness from optic disc photographs correlates with risk of developing primary open-angle glaucoma (POAG) in ocular hypertension.
- Machine-to-machine (M2M) models trained on OCT data accurately estimate RNFL thickness from fundus images, circumventing need for OCT equipment.
- Baseline predicted RNFL thickness and longitudinal thinning rates identified by M2M model independently predict conversion to POAG in OHTS cohort.
- M2M-predicted RNFL thickness offers a noninvasive, accessible biomarker for glaucoma risk stratification and progression monitoring.
Study Background and Disease Burden
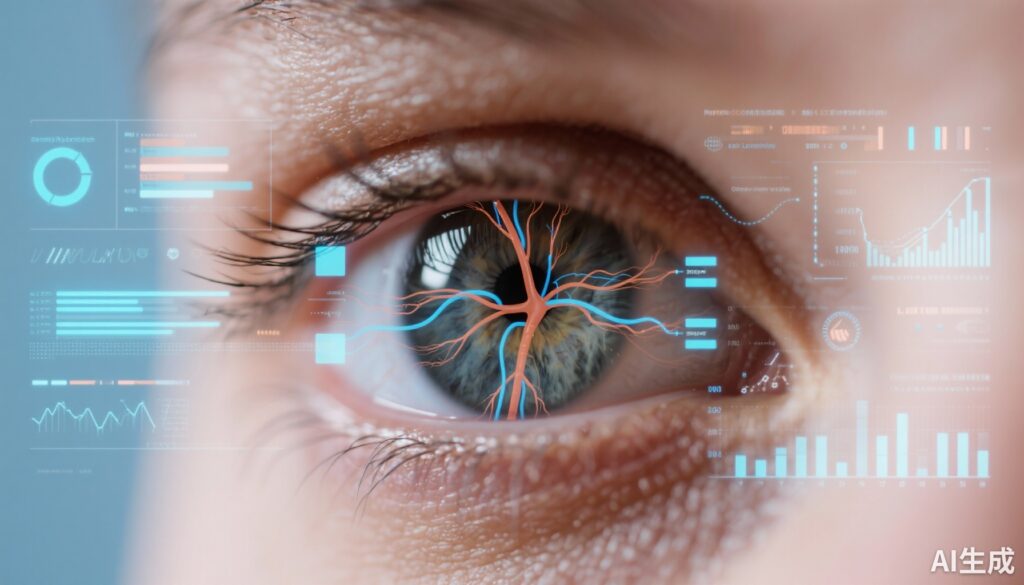
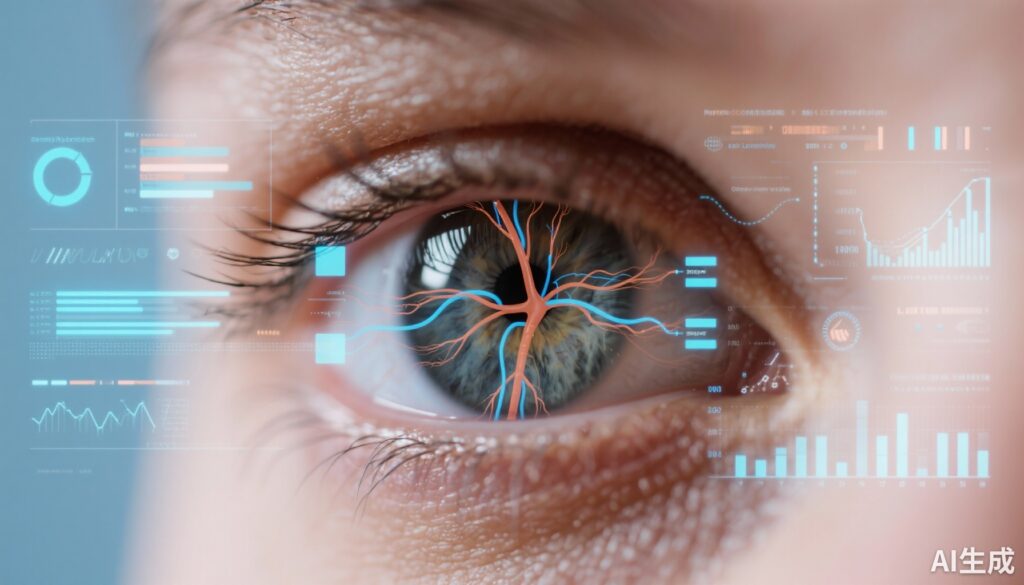
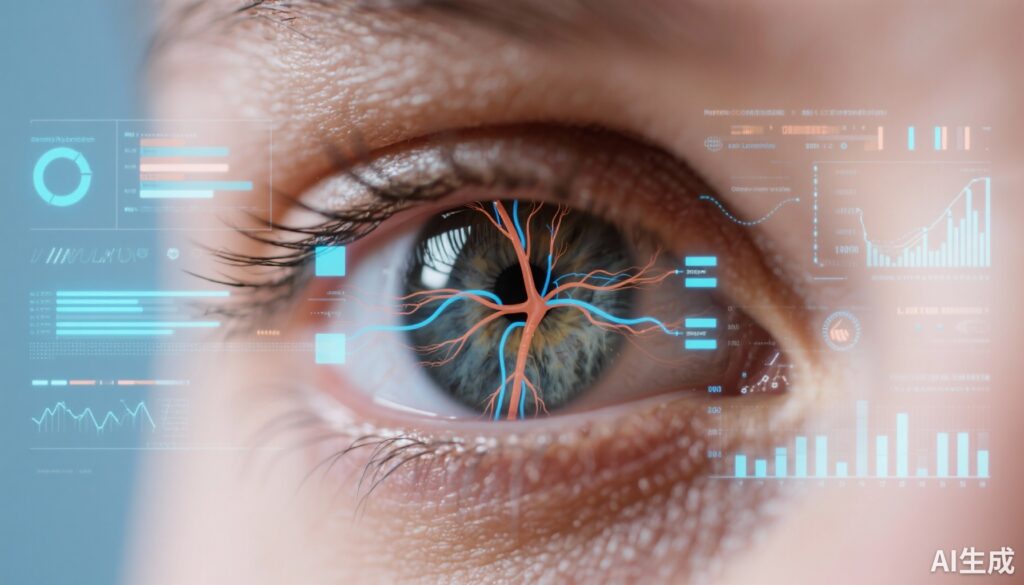
Primary open-angle glaucoma (POAG) is a leading cause of irreversible blindness worldwide, characterized by progressive loss of retinal ganglion cells and their axons, manifesting clinically as thinning of the retinal nerve fiber layer (RNFL) and optic nerve damage. Early detection and monitoring are critical to prevent vision loss. Ocular hypertension, defined as elevated intraocular pressure (IOP) without manifest glaucomatous damage, significantly increases the risk for developing POAG. The Ocular Hypertension Treatment Study (OHTS) established clinical risk factors for conversion but current glaucoma diagnosis and progression monitoring often depend on optical coherence tomography (OCT), which is less accessible globally and costly.
Recent advances in deep learning allow imaging biomarkers such as RNFL thickness to be predicted from conventional optic disc photographs. Such approaches could democratize glaucoma risk assessment by leveraging existing photographic data without reliance on OCT. This study by Liu et al. investigates the ability of an OCT-trained deep learning model (machine-to-machine, M2M) to predict RNFL thickness from ocular hypertensive patients’ optic disc photos and assesses the prognostic value for POAG development.
Study Design
This diagnostic study analyzed data from the OHTS 1 and 2 multicenter trials, involving 3272 eyes from 1636 participants with ocular hypertension but without glaucoma at enrollment. The study period extended from February 1994 to December 2008. Baseline optic disc photographs, demographics, and clinical parameters were included. The M2M deep learning model, trained on OCT-derived RNFL thickness to interpret optic disc photos, generated predicted RNFL thickness values from a large dataset of 66,714 optic disc images.
Primary outcomes focused on the correlation between predicted RNFL thickness and conversion to POAG, assessed using Cox proportional hazards models in univariable and multivariable analyses. Other established POAG risk factors—age, IOP, central corneal thickness, visual field parameters, and cup-to-disc ratio—were also evaluated.
Key Findings
Among 1444 participants analyzed, the mean age was 56.0 years, 57.7% were female. Eyes that developed POAG had significantly lower mean baseline predicted RNFL thickness (94.1 μm) compared to eyes that did not convert (97.1 μm), with a mean difference of 3.0 μm (95% CI, 2.2–3.8; P < .001).
Univariable Cox analysis revealed each 10-μm decrease in predicted RNFL thickness nearly doubled the hazard for conversion to POAG (HR 1.97; 95% CI 1.60–2.42; P < .001). This association remained significant after adjustment for other risk factors (HR 1.83; 95% CI 1.49–2.25; P < .001). Established risk factors such as older age, higher IOP, thinner central corneal thickness, worse visual field pattern standard deviation, mean deviation, and larger cup-to-disc ratio were independent predictors in both analyses.
Importantly, the rate of longitudinal RNFL thinning predicted by the model was a strong risk factor: each 1-μm/year faster predicted loss increased POAG risk sixfold (HR 6.01; 95% CI 3.33–10.64; P < .001).
These findings confirm that baseline and dynamic changes in M2M-predicted RNFL thickness provide prognostic information beyond traditional clinical parameters for glaucoma development in ocular hypertension.
Expert Commentary
This study exemplifies a powerful translational application of artificial intelligence in ophthalmology, utilizing a machine-to-machine approach where deep learning models trained on OCT-measured RNFL thickness generate surrogate quantitative biomarkers from widely available optic disc photographs.
The advantage lies in accessibility—optic disc photographs are a routine, low-cost, and portable imaging modality, especially valuable in settings lacking OCT infrastructure. Predicting RNFL thickness from these can aid both risk stratification and monitoring progression without the need for specialized equipment.
However, some limitations must be considered. The study cohort includes patients from a well-characterized clinical trial with rigorous follow-up; generalizability to diverse populations and real-world clinical settings requires further validation. Additionally, image quality and variability across devices and operators may affect deep learning model performance. The study focused on eyes with ocular hypertension, thus utility in other glaucoma subtypes remains to be established.
Despite these issues, this approach aligns with current trends toward integrating AI algorithms into routine clinical workflows, enhancing early glaucoma diagnosis and personalized management.
Conclusion
The Liu et al. study robustly demonstrates that an OCT-trained deep learning model can accurately predict RNFL thickness from optic disc photographs in ocular hypertensive eyes and that these predictions independently forecast the risk of conversion to primary open-angle glaucoma.
Baseline predicted RNFL thickness and its rate of decline are meaningful biomarkers that complement existing clinical risk factors, offering a noninvasive, widely accessible method to inform glaucoma risk assessment and progression monitoring. These findings expand the potential of AI-powered imaging analytics to improve clinical decision-making and patient outcomes in glaucoma care.
Future research should focus on prospective validation across broader populations and integration into clinical practice platforms for real-time decision support. This innovation represents a paradigm shift toward more accessible, efficient, and quantitative ophthalmic risk stratification using artificial intelligence.