Highlight
1. BO-112, a synthetic dsRNA nanoplexed with polyethylenimine, administered intratumorally, can potentially reverse resistance to anti-PD-1 therapy in advanced melanoma.
2. The SPOTLIGHT-203 phase II trial showed a 25% objective response rate (ORR) in patients with anti-PD-1-resistant melanoma when combining BO-112 with intravenous pembrolizumab.
3. The combination therapy demonstrated a favorable safety profile with manageable grade 3-4 adverse events and no treatment-related deaths.
4. Promising overall survival (OS) outcomes were observed with 54% of patients alive at 24 months, suggesting durable clinical benefit.
Study Background and Disease Burden
Malignant melanoma is a highly aggressive skin cancer with significant morbidity and mortality, especially in advanced or metastatic stages. Immune checkpoint inhibitors targeting programmed cell death-1 (PD-1) have revolutionized melanoma treatment, markedly improving survival. However, a substantial subset of patients exhibits either primary or acquired resistance to anti-PD-1 therapies, leading to limited treatment options and poor prognosis in this population.
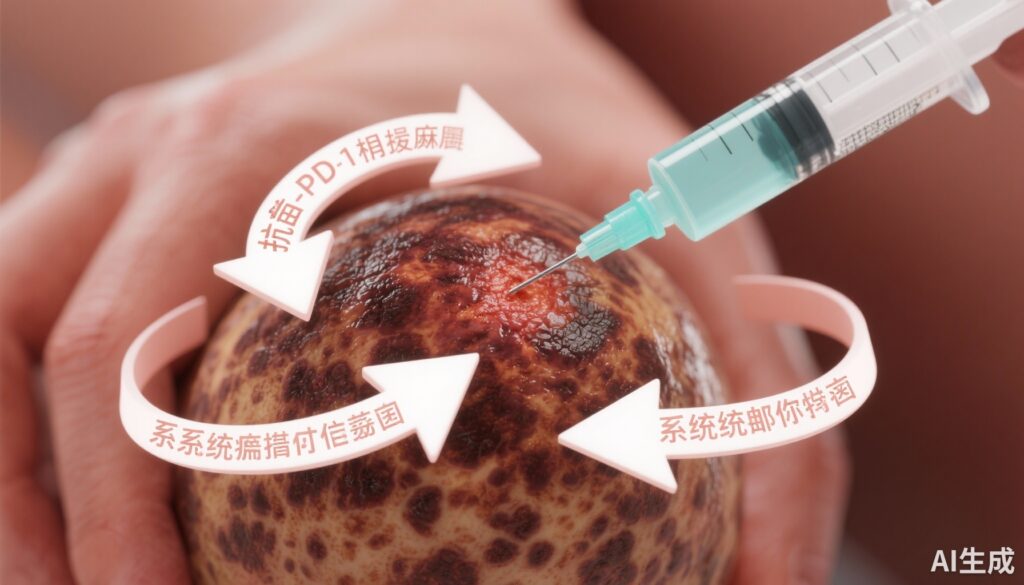
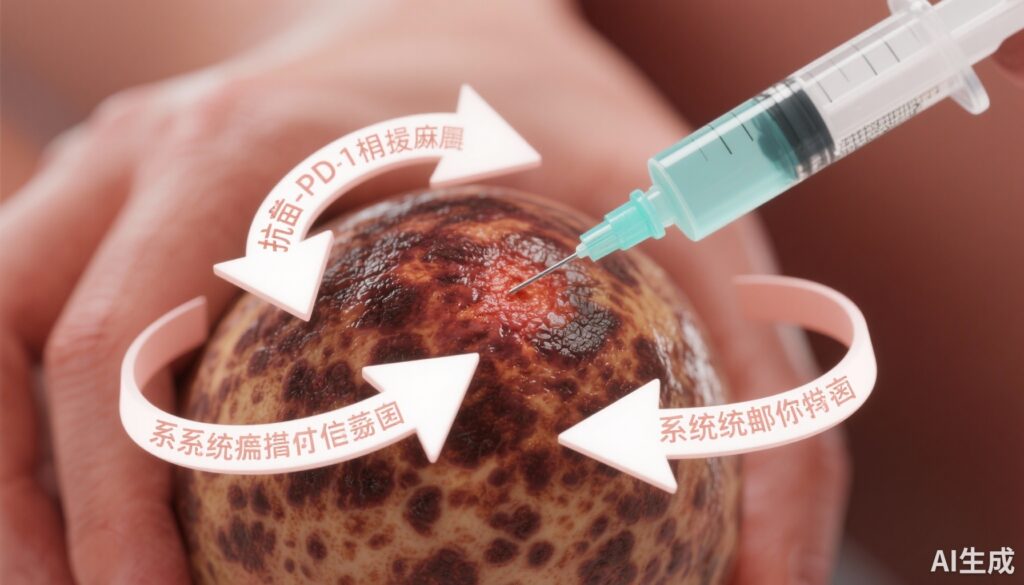
Currently, there is no well-established standard of care for patients with melanoma resistant to anti-PD-1 inhibitors. Novel therapeutic strategies that can overcome or reverse this resistance are urgently needed to improve outcomes. BO-112, a synthetic double-stranded RNA (poly I:C) nanoplexed with polyethylenimine, functions as a Toll-like receptor (TLR) agonist, stimulating innate immune pathways. Intratumoral administration of BO-112 has shown potential to reshape the tumor microenvironment and restore sensitivity to checkpoint blockade in solid tumors, which provides the rationale for combining it with pembrolizumab in this clinical setting.
Study Design
The SPOTLIGHT-203 trial was a multicenter, open-label, phase II clinical study (ClinicalTrials.gov identifier: NCT04570332) investigating the efficacy and safety of intratumoral BO-112 combined with intravenous pembrolizumab in patients with advanced melanoma resistant to prior anti-PD-1 therapy.
A total of 42 patients with confirmed anti-PD-1-resistant melanoma were enrolled. Treatment consisted of intratumoral BO-112 administered weekly for 7 weeks, followed by dosing every 3 weeks, at doses up to 2 mg per injection targeting up to eight injectable lesions. Concurrently, pembrolizumab was administered intravenously at 200 mg every 3 weeks. Therapy was continued until documented progressive disease, unacceptable toxicity, death, or a maximum duration of one year.
The primary endpoint was the objective response rate (ORR) assessed per RECIST 1.1 criteria by independent central radiology review in the modified intention-to-treat population (mITT), comprising patients evaluable for response. The predefined threshold for clinical activity was an ORR of at least 20%. Secondary endpoints included progression-free survival (PFS), overall survival (OS), duration of response (DOR), and safety outcomes.
Key Findings
Efficacy: Among 40 patients evaluable for response (mITT population), the ORR was 25%, comprising 10% complete responses and 15% partial responses. Additionally, 40% of patients achieved stable disease, indicating a disease control rate of 65%.
The median duration of response was not reached at the time of data cutoff (95% CI, 8.3 months to not achieved), suggesting durable responses.
In the intent-to-treat (ITT) population of 42 patients, median progression-free survival was 3.7 months (95% CI, 2.2 to 9.2 months), consistent with outcomes reported in other anti-PD-1-resistant contexts.
Importantly, median overall survival was not reached, with a lower bound of 9.9 months (95% CI, 9.9 to not achieved), and 54% of patients were alive at 24 months, reflecting promising long-term benefit from the combination therapy.
Safety: The combination of BO-112 and pembrolizumab was generally well tolerated. Grade 3-4 adverse events occurred in 38.1% (16 of 42) of patients, but only 9.5% (four patients) were considered related to treatment. There were no reported treatment-related deaths. The manageable toxicity profile supports the feasibility of this therapeutic strategy.
Expert Commentary
The results from the SPOTLIGHT-203 study provide encouraging evidence that intratumoral immune modulation via BO-112 can resensitize melanoma tumors to checkpoint inhibition in patients previously refractory to anti-PD-1 therapy. The observed ORR and disease control rates exceed historical expectations for this difficult-to-treat population. Furthermore, the durable responses and favorable overall survival data underscore the potential for meaningful clinical impact.
Mechanistically, BO-112 engages innate immune sensors such as TLR3, MDA5, and PKR pathways, which may reverse immune exclusion and stimulate type I interferon responses. This immunologic reprogramming of the tumor microenvironment likely synergizes with PD-1 blockade to restore antitumor T cell activity.
Nonetheless, the study is limited by its single-arm design and relatively small sample size, which necessitates confirmation in larger randomized trials. Patient selection and biomarker analyses to identify those most likely to benefit remain areas for further research. Comparisons with other salvage strategies in anti-PD-1-resistant melanoma, such as combination with other immune modulators or targeted agents, will help clarify the optimal treatment algorithms.
Conclusion
The SPOTLIGHT-203 phase II clinical trial demonstrates that intratumoral administration of BO-112 combined with systemic pembrolizumab produces clinically meaningful responses in patients with advanced melanoma resistant to prior anti-PD-1 therapy. The combination met its primary efficacy endpoint with a 25% ORR, exhibited encouraging survival outcomes, and maintained an acceptable safety profile.
These findings suggest that BO-112 may represent a novel immunomodulatory approach to overcoming checkpoint inhibitor resistance and provide a therapeutic option where none is currently established. Future randomized studies and correlative biomarker analyses are warranted to validate and extend these promising results, ultimately improving outcomes for this high unmet need population.
References
Márquez-Rodas I, Dutriaux C, Saiag P, et al. BO-112 Plus Pembrolizumab for Patients With Anti-PD-1-Resistant Advanced Melanoma: Phase II Clinical Trial SPOTLIGHT-203. J Clin Oncol. 2025 Sep;43(25):2806-2815. doi:10.1200/JCO-24-02595.
Topalian SL, Taube JM, Anders RA, Pardoll DM. Mechanism-driven biomarkers to guide immune checkpoint blockade in cancer therapy. Nat Rev Cancer. 2016 May;16(5):275-87.
Judson PL, Sullivan RJ, Niu J, et al. Strategies for Acquired Resistance to Immune Checkpoint Inhibitors in Advanced Melanoma. Cancer Treat Rev. 2023;109:102462.