Highlight
- At one year post-TPIAT, 83% of patients retained islet graft function evidenced by measurable C-peptide levels.
- Pretransplant HbA1c and pediatric age significantly predicted insulin independence at one year.
- Lower baseline HbA1c was strongly associated with better glycemic control (HbA1c <7%) and improved islet graft function.
- White race was also linked to higher odds of achieving target HbA1c levels postoperatively.
Study Background and Disease Burden
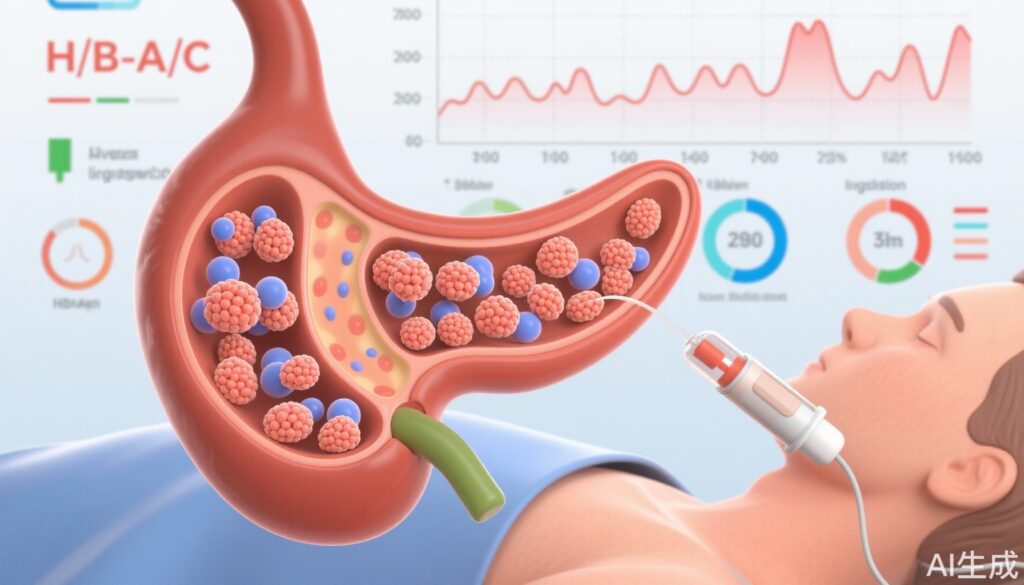
Total pancreatectomy with islet autotransplantation (TPIAT) is a surgical intervention designed to alleviate refractory pain in patients suffering from intractable recurrent acute or chronic pancreatitis. While TPIAT addresses debilitating pain by removal of the pancreas, preserving endocrine function through islet autotransplantation seeks to mitigate diabetes mellitus development—a common and severe complication following total pancreatectomy. Understanding predictors of favorable diabetes outcomes after TPIAT is essential for optimizing patient selection, counseling, and management strategies. Prior data have largely been limited to single-center reports with relatively small sample sizes, underscoring an unmet need for comprehensive multicenter analysis to refine prognostic models.
Study Design
This investigation was a prospective observational multicenter cohort study conducted under the National Institutes of Health-sponsored Prospective Observational Study of TPIAT (POST) program. A total of 384 patients undergoing TPIAT across multiple institutions were enrolled. Participants had a mean age of 29.6 years (standard deviation 17.1) and were predominantly female (61.7%). The study focused on diabetes-related outcomes at one year following surgery, including insulin use status, glycosylated hemoglobin (HbA1c), and islet graft function measured by fasting C-peptide levels. The analysis applied both univariable and multivariable statistical modeling to elucidate factors independently predicting postoperative diabetes parameters.
Key Findings
At one year post-TPIAT, 83% of patients exhibited retained islet function defined by a C-peptide level above 0.3 ng/mL, indicating preserved endogenous insulin secretion. Clinically, 20% of the cohort achieved insulin independence, while 60% maintained HbA1c values below 7%, marking satisfactory glycemic control.
Subgroup analysis revealed that patients who were normoglycemic prior to surgery and children experienced more favorable diabetes outcomes, including higher rates of insulin independence.
Multivariable logistic regression identified several key predictors:
– Pediatric age was associated with more than double the odds of insulin independence at one year (OR 2.3; 95% CI 1.3–4.3) compared to adults.
– Pretransplant HbA1c levels were a potent predictor: every 1% decrease in HbA1c corresponded to a fourfold increase in odds of insulin independence (OR 4.0; 95% CI 1.7–9.1).
– Achieving HbA1c <7% was significantly associated with White race (OR 4.3; 95% CI 1.7–11) and each 1% decrease in baseline HbA1c (OR 2.2; 95% CI 1.1–4.3).
– Islet graft functionality correlated with preoperative fasting C-peptide (OR 2.18; 95% CI 1.42–3.35 per 1 ng/mL increase) and lower baseline HbA1c (OR 1.89; 95% CI 1.18–3 per 1% decrease).
These results underscore the critical role of preoperative glycemic status and endogenous beta-cell activity in post-TPIAT diabetes outcomes.
Expert Commentary
This landmark multicenter cohort study provides robust evidence supporting the prognostic value of preoperative metabolic parameters in predicting diabetes outcomes following TPIAT. The strong association between lower baseline HbA1c and improved postoperative glycemic control and insulin independence suggests that optimizing metabolic status prior to surgery may enhance outcomes. The increased likelihood of insulin independence among pediatric patients aligns with prior reports linking younger age to better islet viability and regenerative capacity.
Notably, disparities observed related to race warrant further investigation, potentially reflecting differential access to care, socioeconomic factors, or biological differences. The reliance on C-peptide as a surrogate of islet graft function is appropriate but future studies incorporating more comprehensive measures of beta-cell function and glycemic variability could augment understanding.
Limitations include the observational design and potential unmeasured confounders such as variation in islet isolation techniques, immunologic factors, and postoperative management protocols across centers. Nevertheless, the large sample size and rigorous multivariable analysis enhance generalizability.
Conclusion
In conclusion, this multicenter cohort study firmly establishes pretransplant HbA1c and pediatric age as powerful predictors of favorable diabetes outcomes after TPIAT. Achieving normoglycemia before surgery significantly increases the probability of insulin independence and preserved islet graft function at one year, emphasizing the importance of metabolic optimization and early intervention. These findings have direct implications for patient counseling and risk stratification, facilitating shared decision-making and individualized treatment planning. Ongoing research should explore strategies to improve preoperative metabolic status, elucidate mechanisms underlying demographic disparities, and refine protocols to maximize islet autotransplant efficacy.
References
1. Witkowski P, Eaton A, Porter S, et al. Predictors of Diabetes Outcomes at 1 Year After Islet Autotransplantation: Data From a Multicenter Cohort Study. Diabetes Care. 2025;48(9):1493-1501. doi:10.2337/dc25-0620.
2. Bellin MD, Sutherland DE, Chinnakotla S, et al. Total pancreatectomy with islet autotransplantation in chronic pancreatitis: Recommendations from PancreasFest. Pancreatology. 2016;16(2):S6-S8. doi:10.1016/j.pan.2016.01.015.
3. Komaya K, Yong B, Matsumoto S, et al. Predicting insulin independence after islet autotransplantation: role of islet yield and pre-transplant beta-cell function. J Clin Endocrinol Metab. 2019;104(1):181-190. doi:10.1210/jc.2018-01032.
4. Rickels MR, Rother KI. Islet transplantation for type 1 diabetes: where do we stand? Endocr Rev. 2019;40(1):3-25. doi:10.1210/er.2018-00167.