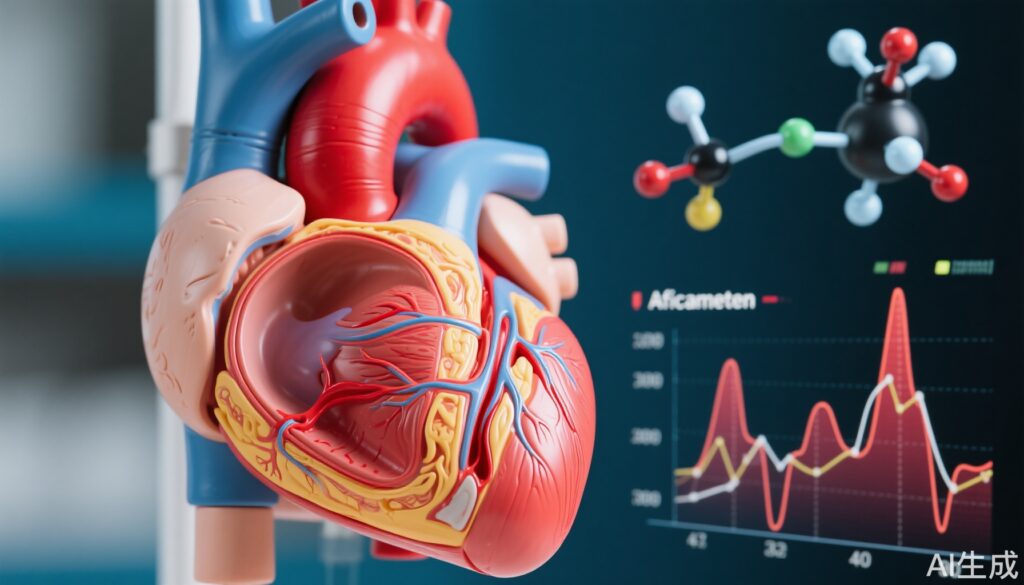
Background and Disease Burden
Obstructive hypertrophic cardiomyopathy (oHCM) is characterized by hypertrophied myocardial tissue causing left ventricular outflow tract (LVOT) obstruction, leading to elevated intracardiac pressures. This obstruction critically contributes to symptoms such as exercise intolerance, dyspnea, chest pain, and syncope, significantly impairing quality of life. Current treatment options include beta-blockers, calcium channel blockers, disopyramide, and invasive septal reduction therapies, yet many patients remain symptomatic. The pathophysiology centers on cardiac hypercontractility. Addressing this mechanism via selective cardiac myosin inhibition represents a novel therapeutic strategy. Aficamten, an oral selective cardiac myosin inhibitor, reduces LVOT gradients by tempering myocardial contractile force without compromising left ventricular ejection fraction (LVEF), thus potentially improving symptoms and functional capacity in oHCM patients.
Study Design
The SEQUOIA-HCM trial is a phase 3, randomized, double-blind, placebo-controlled clinical study evaluating aficamten in adults with symptomatic obstructive hypertrophic cardiomyopathy. A total of 282 patients were randomized in a 1:1 ratio to receive aficamten (starting at 5 mg up to 20 mg daily) or placebo for 24 weeks. Dosing adjustments were guided by echocardiographic assessment of LVOT gradient and LVEF to achieve a Valsalva gradient threshold of <30 mm Hg with LVEF ≥50%. Patients were stratified by symptom severity to assess benefit in milder and more advanced symptomatic subsets. The primary endpoint was change in peak oxygen uptake (peak VO2) by cardiopulmonary exercise testing from baseline to 24 weeks. Ten hierarchical secondary endpoints included changes in Kansas City Cardiomyopathy Questionnaire clinical summary score (KCCQ-CSS), New York Heart Association (NYHA) functional class, LVOT pressure gradients (resting and post-Valsalva), NT-proBNP levels, and eligibility for septal reduction therapy.
Key Findings
The primary analysis demonstrated that at 24 weeks, patients treated with aficamten experienced a statistically significant improvement in peak VO2 compared with placebo (mean increase of 1.8 ml/kg/min vs. 0.0 ml/kg/min; between-group difference 1.7 ml/kg/min; 95% CI, 1.0 to 2.4; P<0.001). This improvement reflects better exercise capacity, a critical clinical outcome.
Secondary endpoints showed consistent benefit, with aficamten recipients experiencing significant improvements in KCCQ-CSS, NYHA functional class, and reductions in LVOT gradients post-Valsalva maneuver. Notably, a greater proportion of aficamten-treated patients achieved LVOT gradients <30 mm Hg, and fewer remained eligible for invasive septal reduction at study end. These benefits were evident as early as 12 weeks.
Subgroup analysis of 118 patients with mild symptoms (NYHA class II and KCCQ-CSS ≥80) revealed that aficamten yielded similar improvements in peak VO2 and symptom relief as seen in patients with more advanced symptoms, supporting efficacy regardless of baseline severity. The magnitude of KCCQ-CSS improvement was somewhat larger in patients with advanced symptoms.
Regarding safety, aficamten demonstrated a favorable profile. Adverse event rates, including atrial fibrillation and worsening heart failure, were comparable between aficamten and placebo groups. A protocol-guided dose titration approach effectively maintained LVEF above 50%, with only 4.9% requiring dose reductions for LVEF declines below this threshold. There were no treatment interruptions or heart failure exacerbations due to LVEF reductions. Aficamten blood levels correlated with dose but remained stable during maintenance, indicating predictable pharmacokinetics.
Expert Commentary
This body of evidence from the SEQUOIA-HCM program establishes aficamten as a promising first-in-class oral therapy that addresses the underlying hypercontractile pathophysiology in obstructive HCM. By selectively inhibiting cardiac myosin, aficamten reduces LVOT obstruction safely without significant negative inotropy or LVEF compromise. The robust improvement in exercise capacity and patient-reported outcomes across symptom severities challenges traditional notions that invasive interventions or more aggressive medical therapy are necessary only in patients with advanced disease. The tolerability profile further supports its suitability for broader clinical use.
Limitations include the relatively short duration (24 weeks) and the fixed titration algorithm based on site echocardiography, which may differ from real-world practice variability. Longer-term data and real-world registries will be critical to confirm durability of effect and safety. Additionally, careful monitoring of LVEF is necessary, given its sensitivity to drug exposure.
From a mechanistic standpoint, aficamten fine-tunes myocardial contractility rather than bluntly suppressing it, which may translate into improved myocardial energetics and remodeling, warranting future investigation.
Conclusion
Aficamten offers a novel, targeted therapeutic option for patients with obstructive hypertrophic cardiomyopathy that significantly improves exercise tolerance, symptoms, and hemodynamic parameters with a reassuring safety profile. Importantly, benefits extend to those with mild symptoms, suggesting early intervention potential. These findings could shift treatment paradigms towards earlier pharmacological modulation of hypercontractility in oHCM. Continued surveillance for long-term outcomes and integration into clinical practice guidelines will be essential to maximize patient benefit.
References
1. Maron MS et al. Aficamten for Symptomatic Obstructive Hypertrophic Cardiomyopathy. N Engl J Med. 2024 May 30;390(20):1849-1861. doi: 10.1056/NEJMoa2401424. PMID: 38739079.
2. Maron MS et al. Efficacy of Aficamten in Patients with Obstructive Hypertrophic Cardiomyopathy and Mild Symptoms: Results from the SEQUOIA-HCM Trial. Eur Heart J. 2025 May 17:ehaf364. doi: 10.1093/eurheartj/ehaf364. PMID: 40380955.
3. Coats CJ et al. Dosing and Safety Profile of Aficamten in Symptomatic Obstructive Hypertrophic Cardiomyopathy: Results From SEQUOIA-HCM. J Am Heart Assoc. 2024 Aug 6;13(15):e035993. doi: 10.1161/JAHA.124.035993. PMID: 39056349; PMCID: PMC11964075.