Highlight
- Fractional flow reserve (FFR)-negative non-culprit (NC) lesions in NSTEMI have less severe stenosis and fewer lipid plaques than those in STEMI.
- Despite these morphological differences, the prevalence of high-risk plaques (HRP) is similar in NSTEMI and STEMI patients.
- Presence of HRP in NC lesions is associated with numerically higher rates of major adverse cardiovascular events (MACE) in both groups over 2 years.
- Findings support further investigation into complete revascularization strategies and therapeutic targeting of HRP in NSTEMI patients.
Study Background and Disease Burden
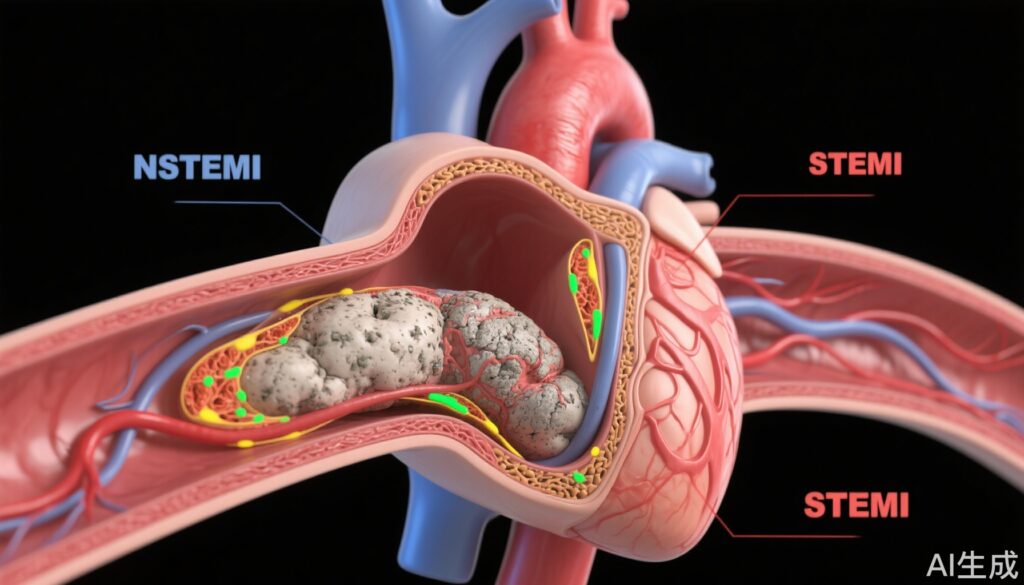
Non-ST-segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI) represent acute coronary syndromes (ACS) with differing pathophysiologies and clinical presentations. While STEMI typically involves abrupt coronary artery occlusion by a culprit lesion, NSTEMI involves partial or transient occlusion. Patients with NSTEMI often have a higher burden of comorbidities and multivessel coronary artery disease, leading to increased risk of recurrent ischemic events.
Despite advances in reperfusion therapy, recurrent events stemming from untreated non-culprit lesions remain a major cause of morbidity and mortality after myocardial infarction (MI). Fractional flow reserve (FFR) guided revascularization has been used to evaluate intermediate lesions, but FFR-negative lesions can still harbor vulnerable high-risk plaque (HRP) features that predispose to future events. Previous studies established the benefit of complete revascularization in STEMI; however, the role and characteristics of HRP in non-culprit lesions of NSTEMI patients remain less well understood.
This study investigates whether non-culprit lesions without ischemia-inducing stenosis (FFR >0.80) in NSTEMI patients exhibit different plaque morphology compared to STEMI and evaluates the prognostic significance of these plaques identified by optical coherence tomography (OCT).
Study Design
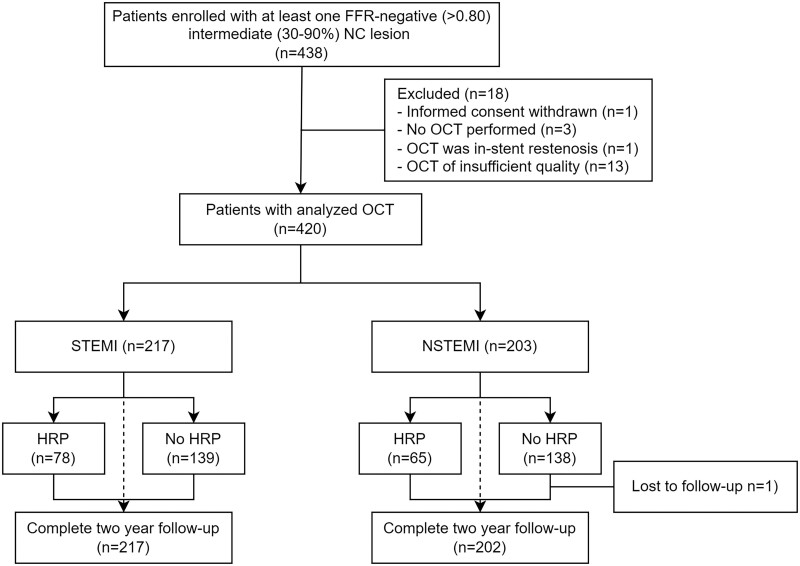
This investigation is a pre-planned subgroup analysis of the multi-center PECTUS-obs study (NCT03857971), a prospective, observational cohort designed to correlate OCT-identified HRP features within FFR-negative intermediate non-culprit lesions to major adverse cardiac events (MACE) post-MI.
A total of 438 patients presenting with NSTEMI or STEMI underwent OCT imaging of all FFR-negative intermediate non-culprit coronary lesions (stenosis visually estimated between 30–90% and FFR >0.80) following successful treatment of the infarct-related artery. The Dragonfly Optis catheter (Abbott Vascular) was used with fluoroscopic guidance. Patients were followed clinically at 1 and 2 years through structured telephone interviews.
The primary endpoint was MACE at 2 years, defined as a composite of all-cause mortality, any non-fatal MI, or unplanned revascularization. Secondary endpoints included individual components of MACE, cardiac death, target-vessel failure/revascularization, and target-lesion failure/revascularization.
Key Findings
Among 420 patients with analyzable OCT data, 203 had NSTEMI and 217 had STEMI presentations. Baseline characteristics highlighted that NSTEMI patients were older (mean 65 vs. 62 years), had more diabetes, hypercholesterolemia, and family history of premature atherosclerosis, consistent with a higher overall cardiovascular risk profile. NSTEMI patients also had higher baseline usage of lipid-lowering therapy and lower LDL cholesterol levels.
In terms of culprit arteries, the circumflex artery was more frequently affected in NSTEMI, whereas the right coronary artery predominated in STEMI. The number and mean FFR values of non-culprit lesions were similar between the groups.
At the lesion level, OCT analysis of 494 FFR-negative NC lesions revealed that NSTEMI patients had significantly larger minimum lumen areas and diameters, and lower percentage area stenosis (approximately 60.5% vs. 64.0%). NSTEMI lesions less frequently contained lipid plaques (70.7% vs. 81.7%) and had shorter lipid length, albeit the prevalence of HRP was not significantly different (29.3% in NSTEMI vs. 32.9% in STEMI).
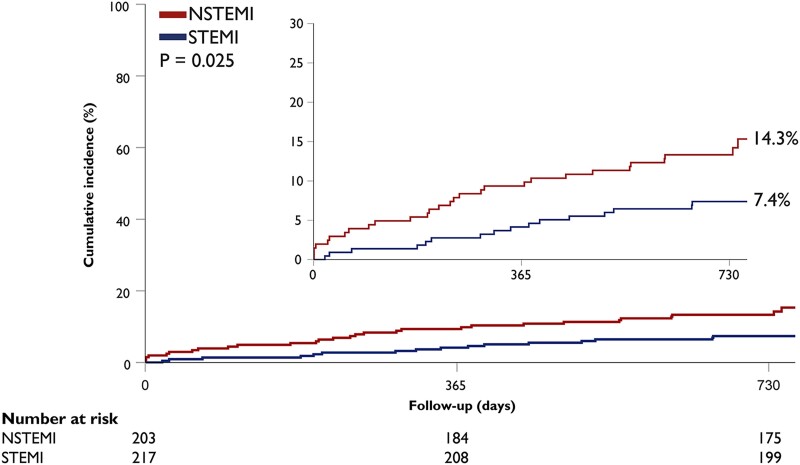
Fig. Two-year MACE. Kaplan–Meier curve for the primary clinical outcome of MACE (composite endpoint of all-cause mortality, non-fatal MI, or unplanned revascularisation) at 2 year follow.
Specific high-risk features such as lipid arc ≥90° were less frequent in NSTEMI, and macrophage accumulation was also lower, but plaque rupture and thrombus prevalence were similar.
Regarding clinical outcomes, 32.0% of NSTEMI and 35.9% of STEMI patients had at least one HRP. At 2-year follow-up, patients with HRP showed numerically higher MACE rates compared to those without HRP in both NSTEMI (20.0% vs. 11.6%; HR 1.83) and STEMI (11.5% vs. 5.0%; HR 2.39) groups, although these differences did not reach statistical significance. There was no significant interaction between clinical syndrome and HRP presence on MACE incidence.
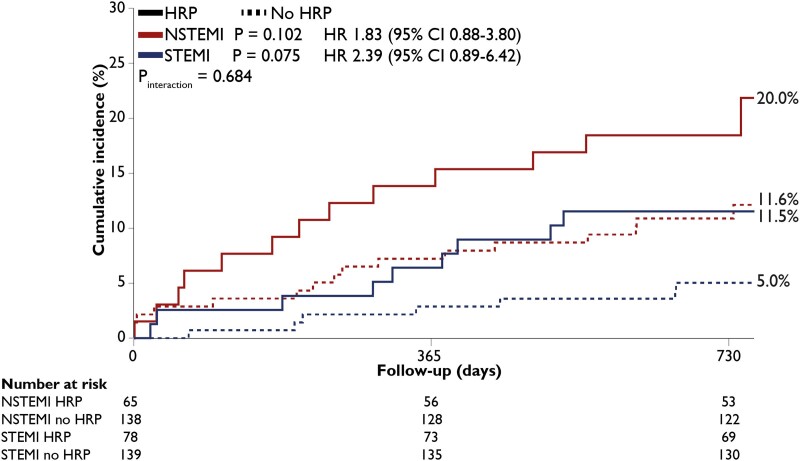
Fig. Two-year MACE and presence of HRP. Kaplan–Meier curve for the primary clinical outcome of MACE (composite endpoint of all-cause mortality, non-fatal MI, or unplanned revascularisation) at 2 year follow according to the presence of a HRP in NSTEMI and STEMI.
Expert Commentary
This study underscores the complexity of coronary artery disease in ACS beyond the culprit lesion, emphasizing that non-culprit lesions, even with FFR >0.80, can harbor features associated with vulnerability and adverse outcomes. The comparable prevalence of HRP between NSTEMI and STEMI non-culprit lesions challenges the assumption that NSTEMI patients have less unstable plaques in non-culprit vessels despite morphological differences such as less lipid burden and larger lumen size.
The findings highlight a potential rationale for expanding the strategy of complete revascularization and targeted medical therapy aimed at stabilizing vulnerable plaques in NSTEMI patients. However, the lack of a statistically significant association with MACE and the observational design call for careful interpretation. Further randomized controlled trials are necessary to determine if interventions targeting HRP in NSTEMI improve clinical outcomes.
Conclusion
FFR-negative non-culprit lesions in NSTEMI patients exhibit less severe stenosis and lower lipid plaque frequency than those in STEMI but have a similar prevalence of high-risk plaque morphology. The presence of HRP correlates with higher numeric MACE rates after MI regardless of clinical presentation. These insights warrant further research into complete revascularization strategies and therapeutic targeting of vulnerable plaques beyond the infarct-related artery in NSTEMI patients.
References
Volleberg RHJA, Mol JQ, Belkacemi A, et al. High-risk plaques in non-culprit lesions and clinical outcome after NSTEMI vs. STEMI. Eur Heart J Cardiovasc Imaging. 2025;26(2):197-206. doi:10.1093/ehjci/jeae289 . PMID: 39512201 ; PMCID: PMC11781827 .