Violence in healthcare settings across the United States poses a serious and growing threat to clinicians, administrative staff, and security personnel. Both urban and rural hospitals are increasingly experiencing incidents of workplace and community violence which cause trauma to healthcare workers and exacerbate operational and financial challenges for hospitals already stretched thin. A recent comprehensive report by the American Hospital Association (AHA) has documented nearly $20 billion in costs related to such violence in 2023, including prevention, treatment, staffing, and infrastructure repair. This article critically examines the clinical and economic impact of workplace violence in hospitals, summarizes the typical patterns and response models employed, and discusses the distinct challenges faced by urban and rural hospitals in addressing this pervasive problem.
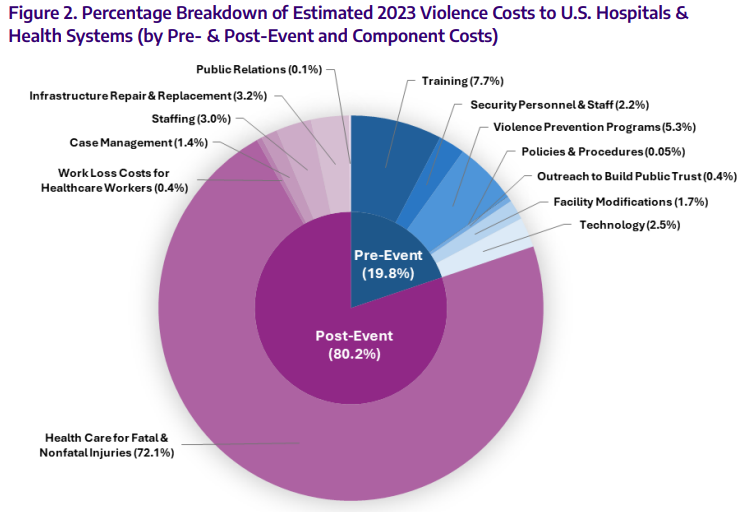
Workplace violence against healthcare workers is recognized as a prominent occupational hazard. The impact ranges from physical injuries to psychological trauma, contributing to burnout and attrition among healthcare providers. The AHA’s 2023 report highlighted a significant financial burden, estimating nearly $20 billion in direct and indirect costs related to violence in hospitals, divided between $3.67 billion on preventive measures and $14.65 billion on post-event expenditures such as healthcare provision, lost workdays, case management, staffing adjustments, and infrastructure repair. Beyond the measurable costs, additional intangible consequences include damage to hospital reputation, compromised recruitment capability, and diminished provider morale—factors difficult to quantify but critical to the health system’s sustainability.
Workplace Violence: Urban and Rural Hospital Settings
Violence in healthcare environments is not restricted to urban or high-population centers; rural hospitals face proportionately similar challenges despite often having fewer documented incidents due to underreporting and less research attention. A study published in the 2023 Online Journal of Rural Nursing and Health Care revealed that rural emergency department nurses confront workplace violence similarly to their urban counterparts. However, rural hospitals typically have more limited resources for prevention and follow-up care, exacerbated by funding constraints. Both urban and rural hospitals must address patient-related social determinants such as untreated mental illness, substance abuse, and socioeconomic stressors, underlying many violent incidents.
Typical Patterns of Violence
Research and expert observation at institutions such as the University of Maryland Medical System (UMMS) reveal a typical escalation pattern: verbal challenges escalate to emotional violence and then can culminate in physical assault against hospital staff. Catrina Bonus, UMMS’ vice president of safety and security, emphasizes the dual need for empathy and clear behavioral expectations during these encounters. UMMS mandates de-escalation training tailored to staff exposure to violence, ranging from online modules for less-affected personnel to hands-on training for frontline workers. Dr. Giora Netzer, UMMS vice president and chief experience officer, highlights the system’s trauma-informed care response model, which aims to establish psychological safety, connection, and diffusion of conflict at every contact point.
Contributing Factors and Rural Challenges
According to Brock Slabach, chief operations officer of the National Rural Hospital Association, emergency departments serve as common venues for workplace violence, especially as they act as de facto social safety nets for individuals facing untreated mental health conditions and other social hardships. Rural patients may arrive with exacerbated medical issues due to barriers in accessing timely care, insurance coverage, and mental health services. Anxiety about healthcare costs among uninsured patients can further escalate tensions, sometimes manifesting as aggression toward staff. Rural hospital staff receive training designed to interrupt violent escalation as early as possible but often face considerable resource challenges compared to urban centers.
Prevention and Intervention Strategies
Evidence supports a multi-tiered, trauma-informed approach to managing and preventing workplace violence across hospital settings. Key strategies include comprehensive staff training in de-escalation techniques, clear behavioral policies communicated empathetically, and psychological support services for affected staff. Security protocols are enhanced with physical infrastructure improvements where feasible. Moreover, integrating community collaboration to improve mental health outreach and reduce social determinants of violence is a critical but underdeveloped facet.
Expert Commentary
Experts acknowledge the complexity of addressing hospital workplace violence due to its socio-behavioral underpinnings. While prevention and training reduce incidents, they do not eliminate the risks created by broader systemic issues such as mental healthcare gaps, rural healthcare underfunding, and social inequities. The AHA’s acknowledgment of intangible costs underscores the need for research into morale, recruitment, and public perception impacts, which may influence long-term hospital viability.
Conclusion
Workplace violence remains a pressing threat to healthcare workers and hospital systems nationally, imposing significant human and financial costs. Both urban and rural hospitals contend with similar patterns of violence and share the imperative of implementing comprehensive prevention and trauma-informed intervention strategies. Addressing the root causes, including mental health and socioeconomic barriers, requires coordinated efforts beyond hospitals themselves. Enhanced funding, particularly for rural hospitals, and ongoing research on psychological and public perception impacts will be essential as healthcare systems strive to protect their workforce and maintain service delivery in an increasingly challenging environment.
References
American Hospital Association. A Comprehensive Assessment of Financial Costs and Other Impacts of Workplace and Community Violence. 2023. Available from: https://www.aha.org/costsofviolence#
Speroni KG, Fitch T, Dawson E, Dugan L, Atherton M. Incidence and Cost of Nurse Workplace Violence Perpetrated by Hospital Patients or Patient Visitors. J Emerg Nurs. 2014;40(3):218-228.
Winstanley S, Whittington R. Aggression Towards Nurses: A Systematic Review of the Literature. J Clin Nurs. 2004;13(1):9-18.
Gacki-Smith J, Juarez AM, Boyett L, Homeyer C, Robinson L, MacLean SL. Workplace Violence Against Nurses: A Literature Review. J Nurs Adm. 2009;39(7/8):340-349.
Online Journal of Rural Nursing and Health Care. Rural Emergency Department Nurses’ Experiences With Workplace Violence. 2023.


