Study Background and Disease Burden
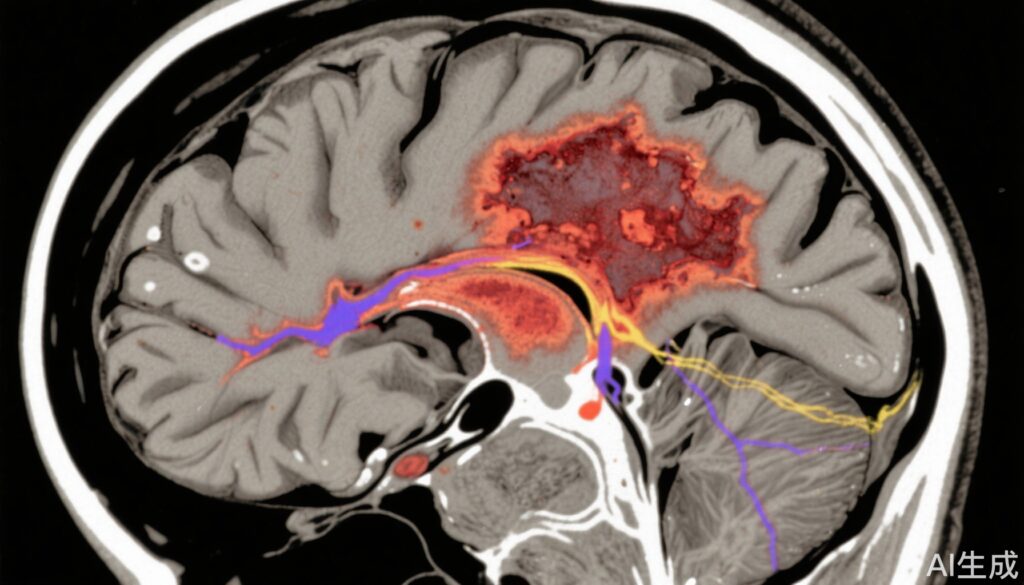
Ischemic stroke caused by large vessel occlusion (LVO) is a leading cause of disability and mortality worldwide. Endovascular thrombectomy (EVT) has dramatically improved clinical outcomes for these patients by restoring perfusion to ischemic brain regions. However, early neurologic deterioration (END) occurs in a significant subset post-EVT, characterized by worsening neurological status within 24 hours. END is associated with poor short- and long-term prognosis. While some cases of END are explained by hemorrhagic transformation or recurrent vessel occlusion, a considerable proportion remains unexplained (unEND), posing challenges for targeted intervention. Understanding the incidence and mechanisms of unEND is critical to improving patient outcomes and tailoring management.
Study Design
This article reviews a post hoc analysis of the ESCAPE-NA1 trial, a large, double-blind, multicenter randomized control trial comparing nerinetide versus placebo in adult patients with anterior circulation LVO treated with EVT. The study analyzed 1063 patients, defining END as an increase of ≥4 points on the NIH Stroke Scale (NIHSS) between the lowest neurological score (baseline or 2-6 hours post-EVT) and the 24-hour assessment. unEND was END without hemorrhagic or thrombotic/thromboembolic events. Multivariable logistic regression was performed to identify variables independently associated with unEND. In a subgroup with baseline CT perfusion (CTP) imaging (n=410), associations between unEND and infarct extension beyond the penumbra (IEBP) were explored, with IEBP indicating a follow-up infarct volume at least 10 mL larger than the initial critically hypoperfused tissue volume.
Key Findings
The analysis revealed that 16.2% of patients experienced END. Of those, 68% (117 patients) had unEND, corresponding to an overall incidence of 11.0%. Variables independently associated with unEND included anesthesia use (adjusted odds ratio [aOR] 7.23; 95% CI 4.63–11.30), older age (aOR 1.02 per year increase; 95% CI 1.01–1.04), and longer onset-to-reperfusion time (aOR 1.02 per 10-minute delay; 95% CI 1.01–1.03). In the CTP subgroup, unEND was strongly associated with IEBP presence (odds ratio [OR] 6.81; 95% CI 2.58–18.01) and larger IEBP volume (OR 1.07 per 10 mL increase; 95% CI 1.01–1.13).
These findings suggest that unEND, affecting about one in ten EVT-treated LVO stroke patients, is linked to factors indicative of brain vulnerability, delayed reperfusion, and anesthesia-related systemic impacts. Importantly, infarct growth beyond the initially hypoperfused penumbra areas likely reflects ongoing ischemic injury or failure of collateral blood flow, highlighting a mechanistic substrate for unEND.
Expert Commentary
The identification of anesthesia use as a strong independent risk factor for unEND raises important clinical considerations regarding procedural sedation and its management during EVT. Older age and delayed reperfusion are well-established risk factors for worse stroke outcomes, consistent in this context of unEND. Mechanistically, infarct extension beyond the initial ischemic penumbra underscores the dynamic nature of cerebral ischemic injury, where reperfusion may not fully salvage tissue and secondary injury pathways can evolve.
While the ESCAPE-NA1 trial focused on the effect of nerinetide, this post hoc analysis did not find therapeutic impact on unEND incidence but provides vital epidemiological and mechanistic data. Limitations include the retrospective nature of the analysis and the relatively modest size of the CTP subgroup, which may affect generalizability. Further research is needed to explore neuroprotective strategies and optimize peri-procedural management to mitigate unEND.
Conclusion
Unexplained early neurologic deterioration after thrombectomy represents a significant clinical challenge, occurring in approximately 10% of treated patients. It is independently associated with anesthesia use, older age, and longer ischemic times. Infarct growth beyond the initial hypoperfused area is a strong mechanistic correlate, reinforcing the importance of timely reperfusion and brain tissue viability monitoring. These insights warrant further prospective investigation to refine EVT perioperative care, including anesthesia protocols and adjunct therapies aimed at reducing unEND and improving overall stroke outcomes.
References
Pensato U, Coutts SB, van Adel B, Chapot R, Puetz V, Demchuk A, Goyal M, Hill MD, Ospel JM; for ESCAPE-NA1. Incidence, Associations, and Mechanisms of Unexplained Early Neurologic Deterioration After Thrombectomy in Stroke Patients. Neurology. 2025 Aug 26;105(4):e213945. doi: 10.1212/WNL.0000000000213945. Epub 2025 Jul 30. PMID: 40737569.