Highlight
– AI-based quantitative computed tomography (AI-QCT) identifies coronary plaque characteristics with sex-specific prognostic significance.
– Although men exhibit higher total plaque volume and high-risk plaque prevalence, women show a substantially higher relative risk of major adverse cardiovascular events (MACEs) per unit plaque burden.
– Key AI-QCT features such as total plaque volume, noncalcified plaque, calcified plaque, and percentage atheroma volume predict outcomes more strongly in women.
– These findings advocate for more aggressive preventive and therapeutic strategies tailored to women’s cardiovascular risk profiles.
Study Background and Disease Burden
Coronary artery disease (CAD) remains a leading cause of morbidity and mortality worldwide. Coronary plaque characteristics, especially their composition and volume, have become critical imaging biomarkers in cardiovascular risk stratification. However, the presence of sex-based differences in coronary atherosclerotic phenotypes and their prognostic implications remain incompletely understood. Historically, women have been underrepresented in cardiovascular studies, and their distinct pathophysiology and clinical presentation often lead to underdiagnosis or undertreatment. Consequently, advanced, sensitive diagnostic approaches that delineate sex-specific coronary plaque features and their associated risks are urgently needed to optimize clinical management and reduce adverse cardiovascular outcomes, including death, myocardial infarction (MI), stroke, unstable angina, and heart failure.
Study Design
This investigation stems from the CONFIRM2 (Coronary CT Angiography Evaluation For Clinical Outcomes: An International Multicenter) Registry, an extensive global, multicenter prospective registry enrolling symptomatic patients with suspected CAD referred for coronary computed tomography angiography (CCTA). A total of 3,551 patients with a mean age of 59±12 years and 49.5% women were included. The study utilized advanced artificial intelligence-based quantitative computed tomography (AI-QCT) to analyze 16 coronary artery disease features, meticulously quantifying total plaque volume, noncalcified plaque, calcified plaque, and percentage atheroma volume across coronary segments.
The primary endpoint was occurrence of major adverse cardiovascular events (MACEs), defined by a composite of death, myocardial infarction, late revascularization, cerebrovascular events, unstable angina, and congestive heart failure. Patient follow-up averaged 4.8±2.2 years, ensuring adequate temporal resolution to assess prognostic associations. Statistical models adjusted for age and established cardiovascular risk factors, and interaction tests were conducted to explore sex differences in predictive value from AI-QCT features.
Key Findings
The study highlights several critical results:
– Event Rates: Among 3,551 patients, overall MACE incidence was 4.8% over the follow-up period, with significantly lower rates in women (3.2%) compared to men (6.1%) (P<0.001).
Table 2. Quantitative AI-QCT Coronary Artery Disease Characteristics
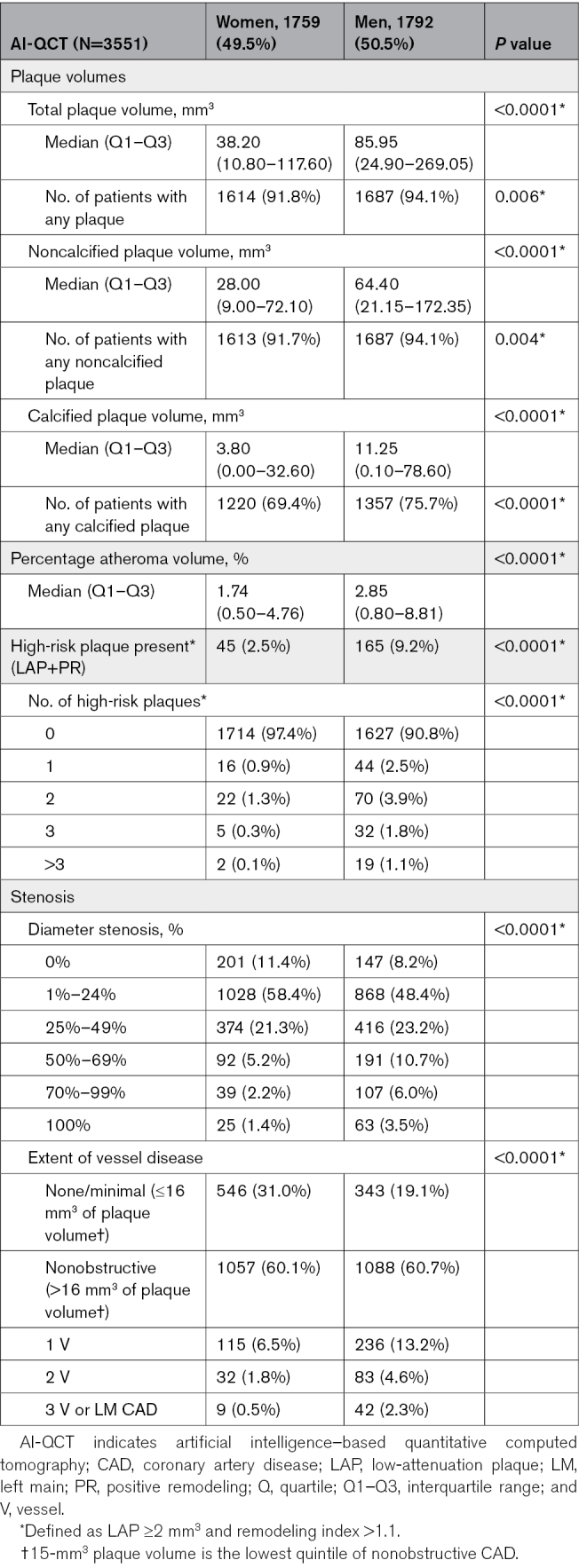
– Plaque Burden and Composition: Men exhibited significantly higher total plaque volume, calcified plaque, noncalcified plaque, and percentage atheroma volume (all P<0.001). High-risk plaques were more prevalent in men (9.2%) than in women (2.5%) (P<0.0001).
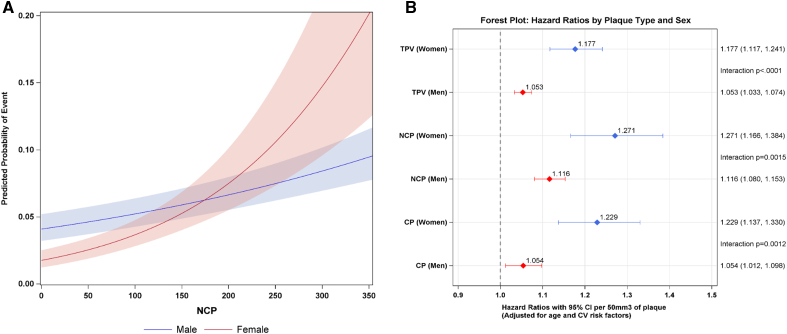
Predicted probability of major adverse cardiovascular event (MACE) in men vs women and forest plot.
– Relative Risk per Plaque Burden Unit: Despite men having greater plaque burden, women demonstrated a notably higher relative risk increase for MACEs per 50-mm3 increase in plaque volume:
* Total plaque volume: 17.7% risk increase in women versus 5.3% in men (Pinteraction<0.001).
* Noncalcified plaque volume: 27.1% risk increase in women versus 11.6% in men (Pinteraction=0.0015).
* Calcified plaque volume: 22.9% risk increase in women versus 5.4% in men (Pinteraction=0.0012).
* Percentage atheroma volume showed similar trends.
– No significant interaction between age and sex was found for MACE prediction (Pinteraction=0.846), indicating differences in relative risk are independent of age.
– Sensitivity Analysis: Restriction to a secondary composite endpoint of death and myocardial infarction did not change the findings, reinforcing the robustness of sex-discordant risk predictions.
These outcomes suggest that while men accumulate more coronary plaque, the presence of a similar or even smaller burden in women corresponds to disproportionately higher adverse cardiovascular risk. This phenomenon may reflect sex-specific pathobiological differences, plaque vulnerability, or differences in microvascular or endothelial function not fully captured by conventional metrics alone.
Expert Commentary
This large-scale multinational analysis leverages cutting-edge AI-QCT technology to illuminate a critical sex disparity in CAD prognostication. It challenges traditional paradigms that equate higher plaque volumes linearly with higher risk across sexes and underscores the need for sex-specific risk algorithms.
Leading cardiovascular imaging experts emphasize that current clinical guidelines should incorporate refined plaque phenotyping, particularly in women, to avoid underestimation of risk. The disproportionate increase in relative risk per plaque volume unit suggests that women may benefit from earlier or more aggressive pharmacologic and lifestyle interventions even when their plaque burden appears modest.
Limitations include potential residual confounding from unmeasured variables, the observational registry design, and the need for external validation in diverse populations. Furthermore, biologic exploration into the mechanisms underpinning the heightened vulnerability in women—such as inflammatory milieu differences or plaque microstructure—remains an important future direction.
Overall, this work provides compelling evidence to inform personalized medicine approaches and highlights AI as a powerful tool to unravel nuanced cardiovascular risks.
Conclusion
The CONFIRM2 Registry study demonstrates that AI-quantified coronary plaque features confer a higher relative risk of major adverse cardiovascular events in women compared to men, despite men having higher absolute plaque volumes. These findings advocate for implementation of sex-specific cardiovascular risk assessment using AI-QCT imaging biomarkers. Clinicians should consider more aggressive preventive therapies and vigilant monitoring in women presenting with coronary atherosclerosis. Future research should explore mechanistic pathways and intervention strategies tailored to modulate sex-specific cardiovascular risk to improve outcomes.
This landmark study underscores the transformative role of artificial intelligence in advancing precision cardiovascular medicine and bridging gender gaps in clinical care.
References
Feuchtner GM, Lacaita PG, Bax JJ, et al. AI-Quantitative CT Coronary Plaque Features Associate With a Higher Relative Risk in Women: CONFIRM2 Registry. Circ Cardiovasc Imaging. 2025 Jun;18(6):e018235. doi:10.1161/CIRCIMAGING.125.018235 IF: 7.0 Q1 . Epub 2025 Mar 31. PMID: 40162910 IF: 7.0 Q1 ; PMCID: PMC12173162 IF: 7.0 Q1 .
[ClinicalTrials.gov Identifier: NCT04279496](https://www.clinicaltrials.gov/ct2/show/NCT04279496)