Highlights
- Flaxseed powder supplementation reduces liver fat and improves lipid metabolism in NAFLD.
- Positive modulation of gut microbiota with increased beneficial bacteria observed.
- Combination with fasting mimicking diet (FMD) offers no added benefit over single interventions in MASLD.
- Improvement in metabolic and inflammatory markers in ulcerative colitis patients with flaxseed supplementation.
Study Background and Disease Burden
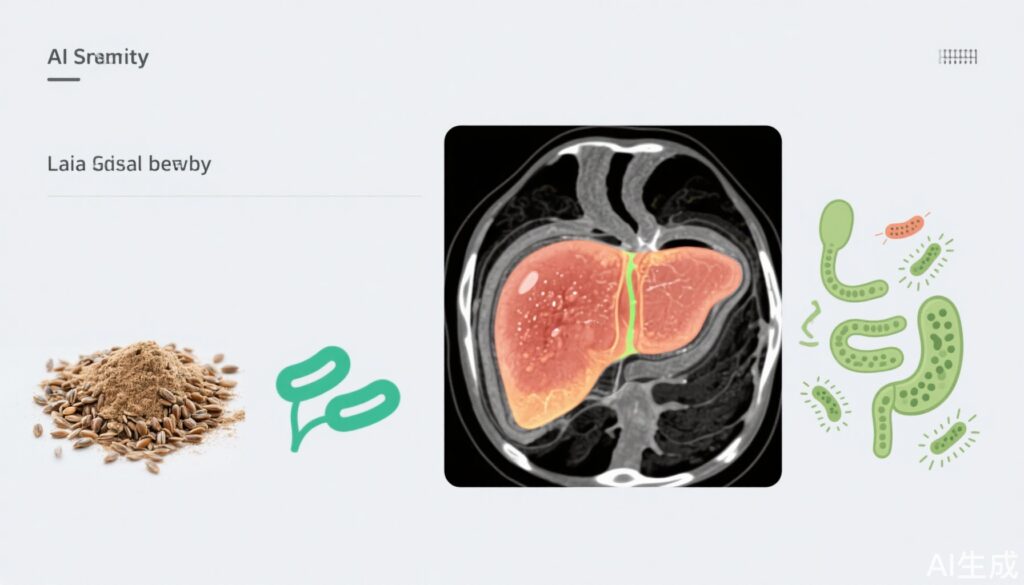
Non-alcoholic fatty liver disease (NAFLD) is a burgeoning public health concern, affecting up to a quarter of the global population. Characterized by excess hepatic fat accumulation without significant alcohol intake, NAFLD is associated with obesity, insulin resistance, and metabolic syndrome. Progressive forms (including metabolic dysfunction-associated steatotic liver disease, MASLD) may lead to cirrhosis, hepatocellular carcinoma, and increased cardiovascular risk. Currently, effective pharmacological treatments are limited, making dietary interventions a critical area of research and clinical practice. Flaxseed, a functional food rich in alpha-linolenic acid, lignans, and dietary fiber, has demonstrated anti-inflammatory, lipid-lowering, and gut microbiota-modulating properties in preclinical models, warranting clinical evaluation.
Study Design
Three recent randomized controlled trials (RCTs) have examined flaxseed supplementation in the context of NAFLD, MASLD, and metabolic syndrome (MetS)-related conditions:
1. **Tian et al., 2025**: A 12-week, parallel-group RCT enrolled 50 NAFLD patients, randomizing them to flaxseed powder (30 g/day before meals plus health education) or control (health education alone). The primary outcome was intrahepatic lipid content measured via MRI-based proton density fat fraction; secondary outcomes included body composition, liver function, and glucolipid metabolism. Gut microbiota analysis was also performed.
2. **Khodadadi et al., 2024**: A 12-week, open-label RCT assigned 100 MASLD patients to one of four groups: control (lifestyle advice), flaxseed (30 g/day), FMD (16 h fasting/day), or flaxseed plus FMD. Outcomes included anthropometric measures, serum biochemistry, liver enzymes, hs-CRP, and hepatic steatosis/fibrosis by elastography.
3. **Morshedzadeh et al., 2021**: In an open-label RCT, 70 ulcerative colitis (UC) patients with mild-to-moderate disease were randomized to flaxseed (30 g/day) or control for 12 weeks. Metabolic and inflammatory parameters were assessed alongside disease activity (SCCAI score).
Key Findings
**1. NAFLD Trial (Tian et al.)**
– Flaxseed group showed significant reductions in liver fat content (primary endpoint), body fat percentage, obesity index, visceral fat area, serum total bilirubin (TBIL), direct bilirubin (DBIL), indirect bilirubin (IBIL), aspartate aminotransferase (AST), total cholesterol (TC), and triglyceride (TG) after 12 weeks (all P < 0.05).
– Increases in serum apolipoprotein A1 (Apo A1) and high-density lipoprotein cholesterol (HDL-C) were observed (P < 0.05).
– Gut microbiota analysis revealed increased Bacteroides and Actinobacteria abundance, decreased Firmicutes/Bacteroidetes ratio, and higher levels of several beneficial genera (Clostridium_sensu_stricto_1, Parasutterella, Lachnospiraceae_NK4A136_group, Eubacterium_xylanophilum_group, Bifidobacterium) versus controls. Coriobacteriaceae_UCG-002 was reduced in the flaxseed group.
– No major adverse events were reported, suggesting a favorable safety profile.
**2. MASLD/FMD-Flaxseed Combination Trial (Khodadadi et al.)**
– All intervention groups (flaxseed, FMD, and combination) showed decreases in triglycerides, total cholesterol, fasting glucose, insulin, hs-CRP, and liver enzymes.
– Hepatic fibrosis scores improved significantly in intervention groups versus control, but hepatic steatosis scores did not differ significantly.
– Importantly, the combination of FMD and flaxseed was not superior to either intervention alone, indicating no additive effect.
**3. Ulcerative Colitis and Metabolic Syndrome Trial (Morshedzadeh et al.)**
– Flaxseed supplementation resulted in significant reductions in serum insulin (p < .001), HOMA-IR (p < .001), triglyceride (p = .001), total cholesterol (p < .001), and increased HDL (p = .008).
– Disease activity (SCCAI score), TNF-α, and CRP improved significantly following flaxseed supplementation.
– No significant changes were found in body weight, BMI, waist circumference, or blood pressure between groups.
**Summary Table: Major Outcomes Across Trials**
| Study | Population | Main Intervention | Primary Benefit | Additional Findings |
|—————-|—————-|——————-|——————————-|————————————|
| Tian et al. | NAFLD | Flaxseed powder | ↓ Hepatic fat, ↑ HDL-C | Gut microbiota modulation |
| Khodadadi et al.| MASLD | Flaxseed/FMD/combo| ↓ Fibrosis, ↓ Metabolic markers| No combo synergy over monotherapy |
| Morshedzadeh et al.| UC/MetS | Flaxseed powder | ↓ Insulin resistance, ↓ CRP | No effect on body composition |
Expert Commentary
The accumulating clinical evidence supports the metabolic and hepatic benefits of flaxseed supplementation in NAFLD and related disorders, echoing preclinical data on its anti-inflammatory and lipid-lowering properties. The modulation of gut microbiota—particularly the enrichment of Bacteroides and Bifidobacterium—suggests a plausible mechanism linking dietary fiber and polyphenol content to enhanced hepatic and metabolic outcomes. However, the lack of additive benefit with fasting mimicking diets (FMD) in MASLD underscores the complexity of dietary interventions in metabolic liver disease and the need for individualized approaches. Limitations include relatively small sample sizes, short intervention durations, and lack of long-term follow-up. The generalizability may be limited to populations with mild-to-moderate disease and stable medication regimens.
Current guidelines for NAFLD management emphasize weight loss, physical activity, and avoidance of hepatotoxic substances. While flaxseed is not yet a recommended therapeutic agent, these findings position it as a promising adjunctive dietary strategy, pending further large-scale studies.
Conclusion
Flaxseed powder supplementation over 12 weeks leads to meaningful improvements in hepatic fat, lipid profiles, inflammatory markers, and gut microbiota composition in NAFLD and related metabolic diseases. Though not synergistic with fasting mimicking diets, flaxseed remains a safe, natural, and effective adjunct for metabolic and hepatic health. Future research should address long-term outcomes, optimal dosing, and integration with other lifestyle interventions.
References
Tian Y, Zhou Y, Liao W, Xia J, Hu Q, Zhao Q, Zhang R, Sun G, Yang L, Li L. Flaxseed powder supplementation in non-alcoholic fatty liver disease: a randomized controlled clinical trial. Food Funct. 2025 Feb 17;16(4):1389-1406. doi: 10.1039/d4fo05847j. PMID: 39878023.
Khodadadi N, Sadeghi A, Poustchi H, Abbasi B, Nilghaz M, Melekoglu E, Yari Z, Hekmatdoost A. Effectiveness of flaxseed consumption and fasting mimicking diet on anthropometric measures, biochemical parameters, and hepatic features in patients with Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): a randomized controlled clinical trial. Nutr Diabetes. 2024 Nov 16;14(1):93. doi: 10.1038/s41387-024-00350-x. PMID: 39550356; PMCID: PMC11569120.
Morshedzadeh N, Rahimlou M, Shahrokh S, Karimi S, Mirmiran P, Zali MR. The effects of flaxseed supplementation on metabolic syndrome parameters, insulin resistance and inflammation in ulcerative colitis patients: An open-labeled randomized controlled trial. Phytother Res. 2021 Jul;35(7):3781-3791. doi: 10.1002/ptr.7081. Epub 2021 Apr 15. PMID: 33856729.