Highlights
- Large, multicenter randomized and observational trials evaluated surgery versus RFA for small hepatocellular carcinoma (HCC).
- No statistically significant difference in 5-year overall survival (OS) or recurrence-free survival (RFS) between surgery and RFA.
- RFA demonstrated a favorable safety profile with no serious adverse events, compared to 3.3% in the surgery group.
- The findings support RFA as an effective, less invasive alternative to surgery for selected small HCC cases.
Study Background and Disease Burden
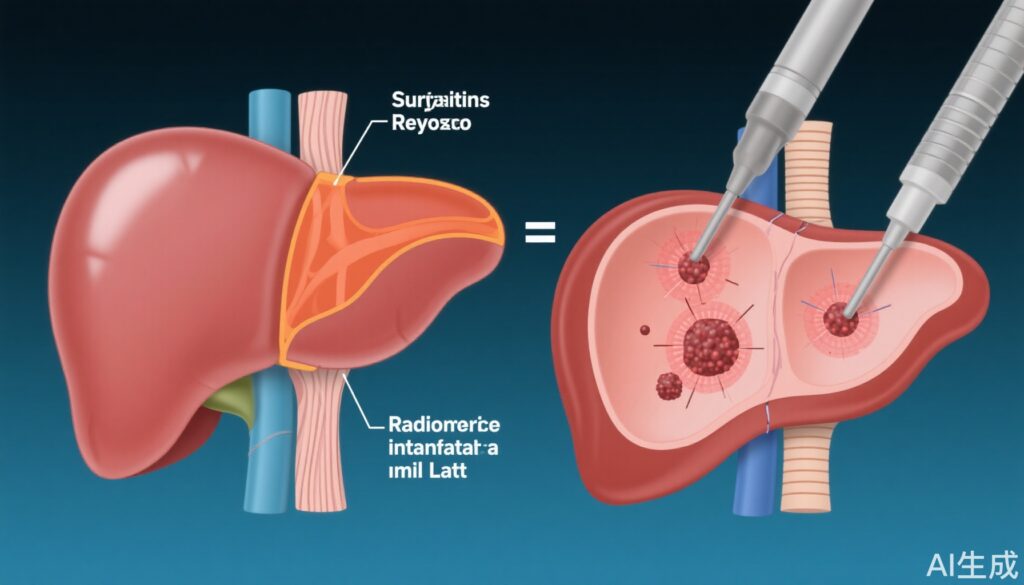
Hepatocellular carcinoma (HCC) is the most common primary liver malignancy and a leading cause of cancer-related mortality worldwide. Early-stage HCC—characterized by one to three lesions with a maximum diameter of ≤3 cm—offers a potentially curable window, commonly treated with surgical resection or local ablative therapies such as radiofrequency ablation (RFA). Surgery has traditionally been considered the gold standard, particularly when liver function is preserved. However, RFA is minimally invasive, repeatable, and associated with shorter hospital stays, prompting debate about its comparative long-term efficacy and safety. Given the increasing incidence of early-detected HCC due to improved surveillance, clarifying the optimal first-line local therapy is a critical unmet need.
Study Design
The SURF trials, conducted across 49 Japanese institutions between 2009 and 2015, comprised two complementary studies:
- SURF-RCT (Randomized Controlled Trial): Patients with ≤3 HCC nodules and largest diameter ≤3 cm were randomized to surgical resection (n=150) or RFA (n=152).
- SURF-Cohort (Nonrandomized Prospective Observational Trial): Eligible patients who declined randomization were enrolled and treated with surgery (n=382) or RFA (n=371).
Co-primary endpoints were recurrence-free survival (RFS) and overall survival (OS). Key demographic and tumor characteristics were well-balanced in the RCT, with 90% presenting with solitary tumors and approximately two-thirds having tumors ≤2 cm.
Key Findings
Randomized Controlled Trial (SURF-RCT):
- Overall Survival (OS): At 5 years, the surgery group had a 74.6% OS rate versus 70.4% in the RFA group (hazard ratio [HR], 0.96; adjusted P = .84), indicating no statistically significant difference.
- Recurrence-Free Survival (RFS): 5-year RFS was virtually identical: 42.9% for surgery and 42.7% for RFA (HR, 0.90; adjusted P = .84).
- Recurrence Patterns and Management: Among those who recurred, most underwent RFA as the retreatment modality, regardless of initial therapy. Only a minority underwent repeat surgery.
- Safety: Serious adverse events occurred in 3.3% of surgical patients, compared to none in the RFA arm, highlighting the procedural safety of ablation in this context.
Observational Cohort (SURF-Cohort):
- Baseline Imbalance: Patients in the cohort study were not randomized, resulting in imbalances in baseline characteristics between groups. Adjusted analyses using inverse probability of treatment weighting were performed.
- Survival Outcomes: After adjustment, no significant differences in OS (P = .77) or RFS (P = .08) were observed between surgery and RFA.
Clinical Implications:
Both trials converge on the conclusion that RFA is non-inferior to surgery in terms of long-term survival and disease control for small HCC, especially when considering the safety and repeatability of ablation.
Expert Commentary
The SURF trials represent a methodologically rigorous effort to address a persistent clinical debate. The robust design, large sample size, and multicenter nature enhance the generalizability of the findings to real-world practice, particularly in East Asian populations where HCC is prevalent.
While surgery may still be preferred for tumors in locations not amenable to ablation or in patients with favorable surgical risk profiles, these results support the adoption of RFA as a first-line modality for small, accessible HCCs. Notably, the use of RFA as a salvage therapy after recurrence was common and effective, indicating the value of a tailored multi-modality approach over the disease course.
As with any study, limitations deserve mention. The majority of patients had solitary, small tumors, which may not reflect outcomes in multifocal or larger HCC. Additionally, the nonrandomized cohort was subject to potential residual confounding despite statistical adjustment. The generalizability to non-Asian populations or centers with less RFA expertise remains to be validated.
Current clinical guidelines from EASL and AASLD already endorse both surgery and ablation for early-stage HCC, with decision-making tailored to tumor characteristics, liver function, and patient preference. The SURF data provide high-level evidence supporting this individualized approach.
Conclusion
The SURF-RCT and SURF-Cohort trials collectively demonstrate that surgical resection does not confer a survival or disease control advantage over radiofrequency ablation in patients with small (≤3 cm), limited-number HCC. RFA offers a less invasive, safe, and effective alternative and can be considered a first-line option in appropriately selected patients. Ongoing research should clarify the role of newer ablation technologies and refine patient selection to maximize outcomes.
References
Kawaguchi Y, Hasegawa K, Kashiwabara K, Okamura Y, Kurosaki M, Kudo M, Shimada M, Yamanaka N, Inomata M, Yamashita T, Tateishi R, Shiina S, Fujishiro M, Matsuyama Y, Omata M, Kokudo N. Surgery Versus Ablation for Hepatocellular Carcinoma: A Randomized Controlled Trial (SURF-RCT Trial) and a Nonrandomized Prospective Observational Trial (SURF-Cohort Trial). J Clin Oncol. 2025 Aug 10;43(23):2628-2638. doi: 10.1200/JCO-24-02030. Epub 2025 Jun 24. PMID: 40554738.
European Association for the Study of the Liver (EASL). EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018 Jul;69(1):182-236.
American Association for the Study of Liver Diseases (AASLD). AASLD practice guidance on the management of hepatocellular carcinoma. Hepatology. 2018 Jan;67(1):358-380.