Highlight
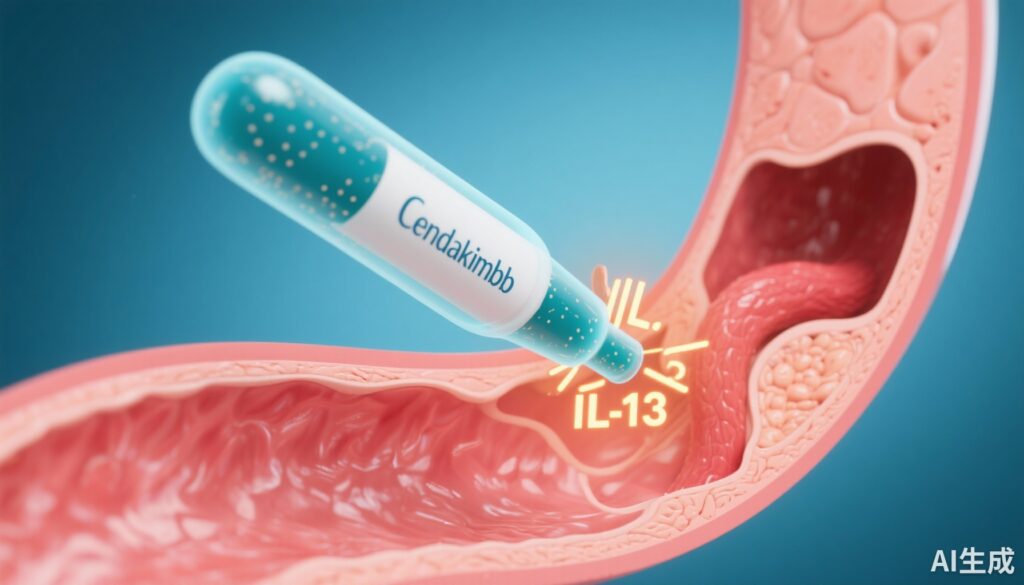
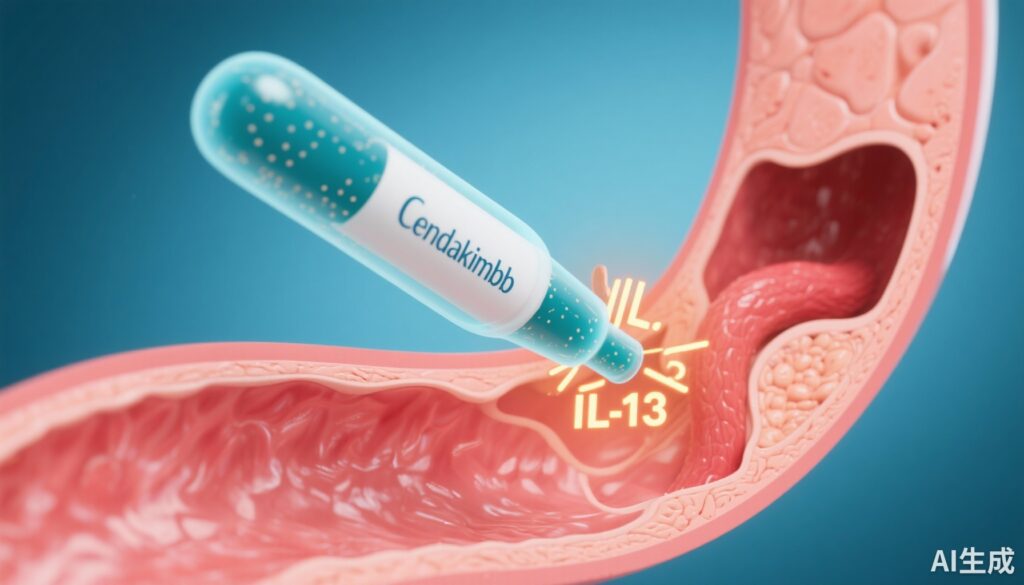
– Cendakimab, a high-affinity monoclonal antibody against IL-13, significantly reduces dysphagia days in EoE patients.
– Achieves histologic response with marked reduction in esophageal eosinophil infiltration.
– Demonstrates improvement in endoscopic severity scores sustained up to 48 weeks.
– Adverse events are common but not dose-limiting, supporting an acceptable safety profile.
Study Background and Disease Burden
Eosinophilic esophagitis (EoE) is a chronic, immune-mediated inflammatory disease characterized by eosinophilic infiltration of the esophageal mucosa, leading to symptoms such as dysphagia and food impaction. The condition primarily involves a type 2 inflammatory response, centrally mediated by the cytokine interleukin 13 (IL-13). EoE prevalence is increasing globally, significantly impacting quality of life and posing therapeutic challenges due to limited treatment options. Current management includes dietary modification and off-label use of corticosteroids, with variable efficacy and potential side effects. There remains an unmet need for targeted, effective, and safe therapies that modify the underlying pathophysiology of EoE.
Study Design
This phase 3, randomized, double-blind, placebo-controlled trial evaluated the efficacy and safety of cendakimab, a monoclonal antibody targeting IL-13, in patients aged 12 to 75 years with diagnosed eosinophilic esophagitis. A total of 430 participants were randomized into three groups: cendakimab 360 mg once weekly for 48 weeks (QW/QW), cendakimab 360 mg once weekly for 24 weeks followed by 360 mg every other week from weeks 24 to 48 (QW/Q2W), or placebo for 48 weeks. The primary endpoints assessed at week 24 included a change from baseline in the number of dysphagia days, measured by a validated patient-reported modified Daily Symptom Diary, and histologic response defined as a peak esophageal eosinophil count of ≤6 per high-power field. Secondary endpoints encompassed endoscopic features assessed via validated scoring methods and safety outcomes. The cendakimab treatment arms were initially analyzed together for the first 24 weeks and subsequently as separate dosing regimens versus placebo for the long-term evaluation.
Key Findings
At week 24, cendakimab administered once weekly significantly reduced dysphagia days compared to placebo, with a least-squares mean change of -6.1 days versus -4.2 days (P<0.001). The histologic response rate favored cendakimab markedly, with 28.6% of treated patients achieving the target eosinophil count compared to 2.2% in the placebo group (P<0.001). Moreover, cendakimab led to a substantial improvement in endoscopic severity scores, with a mean reduction of -5.2 points versus -1.2 points in placebo recipients. These beneficial effects were maintained through week 48 across both cendakimab dosing schedules, demonstrating sustained efficacy.
Safety data indicated that adverse events were reported in 83.8% of patients in the QW/QW group and 84.6% in the QW/Q2W group, compared to 73.4% in the placebo cohort. Most adverse events were mild to moderate and consistent with the drug’s safety profile, without dose-limiting toxicities observed. The tolerability supports cendakimab’s application in a broad age range including adolescents and adults.
Expert Commentary
This robust phase 3 study provides compelling evidence that targeting IL-13 with cendakimab effectively addresses fundamental disease processes in EoE, resulting in both symptomatic relief and mucosal healing. The dual blockade of IL-13 receptor alpha 1 and alpha 2 by cendakimab offers a mechanistic advantage in modulating the type 2 inflammatory cascade that drives eosinophilic infiltration and esophageal dysfunction.
While dietary and corticosteroid therapies remain standard, cendakimab’s targeted approach represents a paradigm shift toward biologic therapy in EoE. Nevertheless, longer-term real-world data and direct comparisons with other emerging biologics such as dupilumab are warranted to fully define its positioning.
Potential limitations include the relatively modest histologic response rate (~29%) at 24 weeks, indicating that while cendakimab benefits a meaningful subset of patients, combination therapies or alternative dosing strategies might optimize outcomes. Additionally, the high incidence of adverse events emphasizes the need for vigilant monitoring, though the lack of dose-limiting toxicity is reassuring.
Conclusion
Cendakimab is a promising targeted therapy for adolescents and adults with eosinophilic esophagitis, significantly improving clinical symptoms, histologic inflammation, and endoscopic disease severity. The sustained efficacy through 48 weeks alongside an acceptable safety profile supports its role as a novel therapeutic option addressing the unmet needs in EoE management. Future research should explore longer term outcomes, comparative effectiveness, and integration into treatment algorithms to enhance patient benefit.
References
Dellon ES, Charriez CM, Zhang S, et al. Cendakimab in Adults and Adolescents with Eosinophilic Esophagitis. NEJM Evid. 2025 Oct;4(10):EVIDoa2500095. doi: 10.1056/EVIDoa2500095. Epub 2025 Sep 23. PMID: 40985784.
Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128(1):3-20.e6. doi:10.1016/j.jaci.2011.02.040
Dellon ES, Hirano I. Epidemiology and natural history of eosinophilic esophagitis. Gastroenterology. 2018;154(2):319-332.e3. doi:10.1053/j.gastro.2017.07.045
AI Thumbnail Prompt
“Illustration of monoclonal antibody cendakimab blocking IL-13 interaction with esophageal tissue, symbolizing targeted therapy for eosinophilic esophagitis”