Study Background and Disease Burden
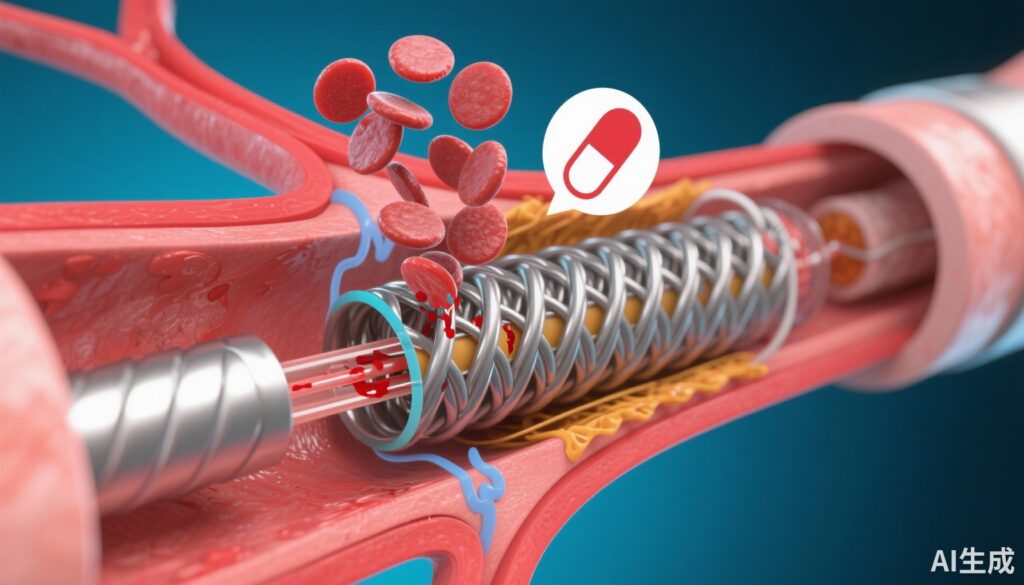
Percutaneous coronary intervention (PCI) with stent implantation is a cornerstone therapy for coronary artery disease, particularly in patients presenting with acute coronary syndrome (ACS). Current guidelines recommend dual antiplatelet therapy (DAPT), typically aspirin plus a P2Y12 receptor inhibitor such as prasugrel, to prevent thrombotic complications like stent thrombosis. However, bleeding complications associated with DAPT, especially within the initial month post-PCI, remain a significant clinical challenge. These complications are accentuated in patients at high bleeding risk (HBR), leading to increased morbidity and mortality.
Recent interest has emerged in exploring aspirin-free antiplatelet strategies to mitigate bleeding without compromising ischemic protection. The rationale is that potent P2Y12 inhibitor monotherapy could maintain antithrombotic efficacy while reducing bleeding risk inherent to aspirin use. Yet, robust evidence from randomized trials confirming the safety and efficacy of such an approach in high-risk populations, including ACS and HBR patients, has been lacking.
Study Design
The STOPDAPT-3 trial was a prospective, randomized, open-label trial enrolling 6,002 patients with ACS or HBR immediately prior to PCI. Participants were randomized to receive either:
1. Prasugrel monotherapy (3.75 mg daily) following a 20 mg loading dose.
2. Standard DAPT consisting of aspirin (81–100 mg daily) plus prasugrel (3.75 mg daily) after the same loading dose.
Key inclusion criteria targeted a population with elevated ischemic and bleeding risk, making the study’s findings especially relevant for real-world clinical practice. The trial employed coprimary endpoints evaluated at 1 month post-PCI:
– Major bleeding events defined by Bleeding Academic Research Consortium (BARC) type 3 or 5, assessed for superiority.
– Cardiovascular events composite (cardiovascular death, myocardial infarction, definite stent thrombosis, ischemic stroke), assessed for noninferiority with a 50% relative margin.
This design allowed the investigation of whether aspirin omission could reduce bleeding without compromising ischemic protection during the vulnerable early post-PCI period.
Key Findings
Of the 5,966 patients analyzed (2,984 no-aspirin; 2,982 DAPT), baseline characteristics were well balanced: mean age 71.6 years, 76.6% male, and 75.0% presenting with ACS. Prior to randomization, a notable proportion had received aspirin (alone 21.3%, with P2Y12 inhibitor 6.4%), oral anticoagulants (8.9%), or intravenous heparin (24.5%). Protocol adherence was high in both arms (88% at 1 month).
The principal results at 1 month included:
– Major bleeding rates were similar: 4.47% in the aspirin-free group vs. 4.71% in DAPT group (hazard ratio, 0.95; 95% CI, 0.75–1.20; Psuperiority=0.66), indicating no superiority of aspirin omission in reducing early major bleeding.
– Cardiovascular event rates were 4.12% vs. 3.69% respectively (hazard ratio, 1.12; 95% CI, 0.87–1.45; Pnoninferiority=0.01), demonstrating noninferiority of prasugrel monotherapy with respect to ischemic outcomes.
– No significant differences were observed in net adverse clinical events or individual components of the cardiovascular composite endpoint.
Despite these neutral primary outcomes, safety signals emerged:
– The aspirin-free group experienced higher rates of unplanned coronary revascularization (1.05% vs. 0.57%, HR 1.83, 95% CI 1.01–3.30).
– Subacute definite or probable stent thrombosis occurred more frequently in the aspirin-free group (0.58% vs. 0.17%, HR 3.40, 95% CI 1.26–9.23).
These findings raise concerns regarding thrombotic risk with aspirin omission early post-PCI.
Expert Commentary
STOPDAPT-3 addresses a critical question in antiplatelet management post-PCI, particularly for patients with competing bleeding and ischemic risks. The lack of bleeding reduction contrasts with the initial hypothesis that aspirin exclusion would diminish hemorrhagic complications. This may reflect the potent antiplatelet effect of low-dose prasugrel monotherapy being insufficient alone to prevent certain thrombotic events, underscored by increased stent thrombosis in the aspirin-free arm.
The trial’s high adherence rates and broad inclusion criteria enhance generalizability. Nevertheless, the open-label design and 1-month follow-up limit longer-term safety assessment. Additionally, the trial utilized a low prasugrel dose (3.75 mg/day) typical in East Asian populations, which may limit extrapolation to other demographic groups.
Guidelines currently recommend DAPT for 6 to 12 months post-ACS PCI. Findings from STOPDAPT-3 suggest that aspirin discontinuation immediately after PCI may be premature, especially among high-risk thrombotic patients. Future studies might explore tailored de-escalation strategies, balancing ischemic and bleeding risks more precisely.
Conclusion
The STOPDAPT-3 randomized trial demonstrates that an aspirin-free strategy using low-dose prasugrel monotherapy does not reduce major bleeding within the first month after PCI compared to conventional DAPT but is noninferior for short-term cardiovascular outcomes. Importantly, the aspirin-free approach was associated with increased risks of unplanned coronary revascularization and stent thrombosis, indicating caution in omitting aspirin early after coronary stenting, particularly in ACS or high bleeding risk patients.
These results support continuation of DAPT with aspirin and prasugrel during the initial post-PCI period until further evidence clarifies optimal antiplatelet regimens balancing bleeding and ischemic risks.
References
1. Natsuaki M, Watanabe H, Morimoto T, et al. An Aspirin-Free Versus Dual Antiplatelet Strategy for Coronary Stenting: STOPDAPT-3 Randomized Trial. Circulation. 2024;149(8):585-600. doi:10.1161/CIRCULATIONAHA.123.066720.
2. Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease. Eur Heart J. 2018;39(3):213-260.
3. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease. J Am Coll Cardiol. 2016;68(10):1082-1115.
4. Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736-2747.