Highlight
- This landmark randomized controlled trial (RCT) is the first to directly compare urgent surgery versus fibrinolytic therapy (FT) using low-dose, slow-infusion tissue plasminogen activator (t-PA) for symptomatic left-sided prosthetic valve thrombosis (PVT).
- The study found no significant difference in complete clinical response between urgent surgery and fibrinolysis but reported significantly higher composite adverse events — particularly death — associated with surgery.
- Fibrinolytic therapy, while safer, was associated with a notable proportion of residual valve dysfunction post-treatment.
Study Background and Disease Burden
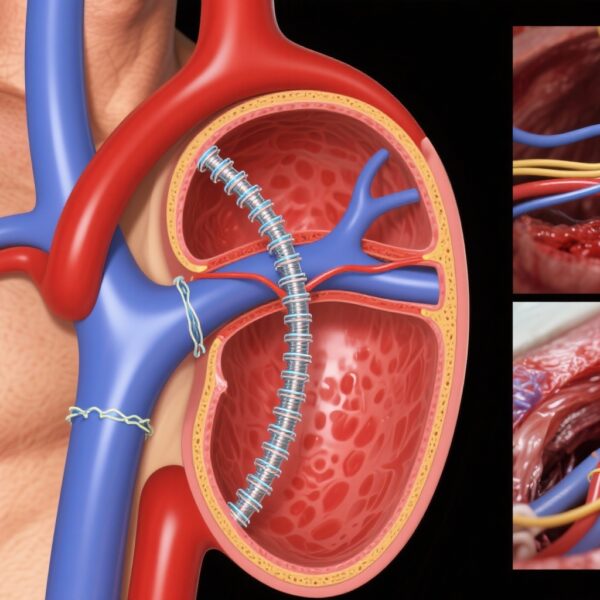
Prosthetic valve thrombosis is a severe complication affecting patients with mechanical heart valves, occurring most frequently on the left-sided (mitral or aortic) valves. It is particularly prevalent in low-resource settings where challenges in patient follow-up, anticoagulation management, and emergent care contribute to increased incidence. PVT can manifest as obstructive valve dysfunction causing heart failure symptoms and systemic embolization, demanding urgent intervention.
Current standard treatments include urgent surgery to replace or repair the thrombosed valve or fibrinolytic therapy aimed at thrombus dissolution. While urgent surgery offers definitive mechanical resolution, it carries significant procedural risks. Fibrinolytic therapy is less invasive but raises concerns for incomplete resolution and bleeding complications. Until now, treatment choices have rested primarily on observational data and expert consensus, lacking robust randomized comparative evidence.
Study Design
This single-centre, open-label randomized controlled trial enrolled 79 patients over six years presenting with symptomatic left-sided mechanical PVT. Patients were randomized 1:1 to urgent surgery or fibrinolytic therapy with low-dose, slow-infusion t-PA.
Inclusion criteria emphasized symptomatic patients with echocardiographic evidence confirming obstructive thrombus on mitral or aortic prostheses. The primary efficacy outcome was “complete clinical response,” defined as hospital discharge with fully restored valve function without major complications.
The prespecified primary safety outcome was a composite measure comprising death, non-fatal stroke, non-fatal major bleeding, or systemic embolism at hospital discharge. Outcome assessment was blinded to treatment allocation to maximize objectivity.
Key Findings
Among 79 randomized patients (39 surgery, 40 FT), 72% had thrombosed mitral prostheses, and 43% were in NYHA functional class III/IV, demonstrating a high-risk cohort.
In surgery-assigned patients, only 32 underwent the procedure, with 53% having surgery within 48 hours, highlighting logistic challenges. All FT patients received the intended t-PA regimen.
Intention-to-treat analysis revealed no statistically significant difference in complete clinical response: 25/39 (64%) in surgery vs 29/40 (73%) in FT (OR 1.22, 95% CI 0.46-3.19; P=0.689). However, the composite safety outcome occurred significantly more often post-surgery (OR 5.14, 95% CI 1.28-20.5; P=0.021), primarily due to higher mortality (7/39 vs 1/40; P=0.035).
Importantly, 25% of FT patients had residual valve dysfunction on discharge, representing incomplete thrombus resolution or valve impairment post-treatment.
Expert Commentary
This pioneering RCT challenges the traditional preference for urgent surgery in left-sided PVT, particularly in resource-limited environments. The higher mortality and complications associated with surgery underscore real-world risks, including procedural delays and perioperative morbidity.
The low-dose, slow-infusion t-PA protocol appears to offer a safer alternative, with comparable success rates but a propensity for residual valve dysfunction that may necessitate close follow-up and possible reintervention. This supports a more individualized treatment approach balancing patient stability, surgical risk, and available expertise.
Limitations include single-centre design and potential selection biases, with some crossover reducing treatment purity. Nonetheless, blinding outcome assessment strengthens the validity of findings. Further multicentre trials should explore confirmatory evidence and optimal fibrinolytic regimens.
Conclusion
For symptomatic left-sided prosthetic valve thrombosis, urgent surgery does not confer superior efficacy over fibrinolytic therapy but is linked to significantly higher complication rates, especially mortality. Fibrinolytic therapy with low-dose, slow-infusion t-PA, while safer, leaves a subset with residual valve dysfunction requiring continued surveillance.
These findings advocate reconsideration of treatment paradigms, particularly in settings where surgical resources are constrained. Clinicians should weigh risks and benefits carefully, tailoring therapy to patient profiles and infrastructure. Future research should refine fibrinolytic protocols and investigate longitudinal outcomes to optimize care strategies.
References
Karthikeyan G, Rajashekar P, Devasenapathy N, Biswas S, Kidambi B, Singal A, Mantoo MR, Soni M, Purohit G, Hote MP, Singh S, Velayoudam D. Urgent surgery vs fibrinolytic therapy for left-sided prosthetic valve thrombosis: a randomized trial. Eur Heart J. 2025 Sep 8;46(34):3373-3381. doi: 10.1093/eurheartj/ehaf391. PMID: 40574603.
Vahanian A, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561–632.
Zoeckler T, et al. Management of prosthetic valve thrombosis with thrombolytic therapy: systematic review. Eur Heart J. 2010;31:1481–1488.