Study Background and Disease Burden
Coronary artery disease (CAD) involving the left main coronary artery or multiple vessels represents a significant clinical challenge due to its complexity and heightened risk of adverse cardiovascular events. Traditionally, coronary artery bypass grafting (CABG) has been considered the gold standard intervention for such complex CAD, consistently demonstrating superior long-term outcomes compared to conventional percutaneous coronary intervention (PCI). Multiple landmark trials have reported better survival rates and fewer major adverse cardiac and cerebrovascular events (MACCE) associated with CABG in patients with left main or 3-vessel disease.
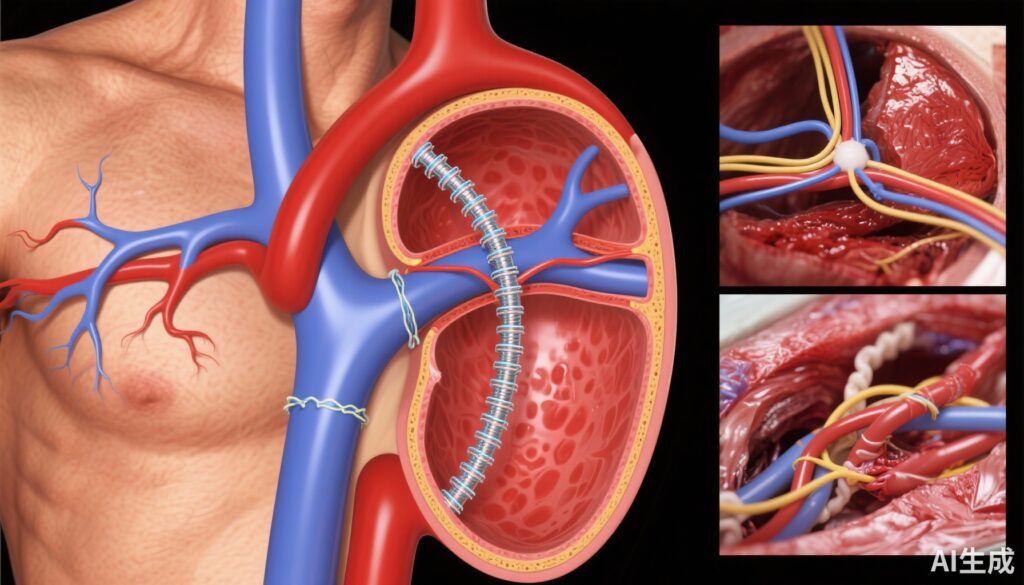
However, advances in PCI techniques and adjunctive technologies have prompted re-evaluation of this paradigm. In particular, the use of intravascular imaging (IVI)—such as intravascular ultrasound (IVUS) or optical coherence tomography (OCT)—to guide PCI has improved procedural optimization and stent deployment precision. Yet, whether IVI-guided PCI can close the outcome gap with CABG in this high-risk population remains incompletely understood. This question is clinically significant given the less invasive nature of PCI and the potential for reduced perioperative morbidity.
Study Design
The study combined data from the RENOVATE-COMPLEX-PCI randomized trial and a large institutional registry from Samsung Medical Center. Overall, 6,962 patients with left main or 3-vessel CAD were analyzed. Patients were categorized into three groups based on intervention: 848 underwent IVI-guided PCI; 987 underwent angiography-guided PCI without IVI; and 5,127 underwent CABG.
The primary endpoint was a composite of all-cause mortality, nonfatal myocardial infarction, or stroke assessed at 3 years post-procedure. Propensity score matching was utilized to adjust for baseline differences between IVI-guided PCI and CABG cohorts to enable balanced comparative analysis.
Key Findings
The study confirmed that overall, PCI (combining both IVI-guided and angiography-guided) was associated with a higher risk of the primary composite endpoint compared to CABG (13.3% vs 10.8%; hazard ratio [HR]: 1.23; 95% confidence interval [CI]: 1.05-1.44; P = 0.013).
Importantly, the IVI-guided PCI subgroup demonstrated a comparable risk of adverse events to the CABG group (8.7% vs 10.8%; HR: 0.77; 95% CI: 0.59-1.01; P = 0.058), approaching statistical significance favoring IVI-guided PCI. Propensity score-matched analysis reinforced this observation, showing nearly identical event rates between IVI-guided PCI and CABG (9.5% vs 9.4%; HR: 0.98; 95% CI: 0.69-1.40; P = 0.914).
In contrast, angiography-guided PCI without intravascular imaging was associated with worse outcomes compared to CABG, highlighting the clinical benefit of IVI guidance. Secondary outcomes and safety profiles were consistent with these observations, endorsing the hypothesis that image-guided PCI optimizes procedural success and reduces ischemic complications.
Expert Commentary
These findings provide compelling real-world and randomized data to suggest that IVI-guided PCI may narrow the clinical outcome disparity historically observed between PCI and CABG for left main or 3-vessel CAD. By enhancing lesion assessment, stent sizing, and deployment accuracy, intravascular imaging likely contributes to improved vessel patency and less restenosis.
While the study is hypothesis-generating and observational elements limit causal inferences, its large sample size and robust propensity matching enhance its relevance. Experts underscore the evolving role of intravascular imaging as a standard adjunct in complex CAD intervention.
Current guidelines recommend considering CABG as first-line in extensive multi-vessel disease, but these data suggest an individualized approach incorporating IVI-guided PCI may be a viable alternative, especially for patients with prohibitive surgical risk. Further large-scale randomized controlled trials with longer follow-up are warranted to confirm mortality and quality-of-life differences.
Conclusion
In patients with left main or 3-vessel coronary artery disease, PCI guided by intravascular imaging demonstrates clinical outcomes comparable to CABG over a 3-year horizon, contrasting with inferior results seen with angiography-guided PCI alone. This evidence supports integration of IVI into PCI procedural standards for complex CAD and suggests a potential shift in revascularization strategies could be considered, balancing efficacy and patient-specific factors.
Optimizing personalized coronary revascularization requires continued research, but IVI-guided PCI emerges as a promising modality that may expand treatment options and improve outcomes for patients with complex coronary anatomy.
References
1. Lee SY, Cho YH, Sung K, Kim WS, Lee SJ, Kwon W, Lee JY, Lee SH, Shin D, Lee SY, Kim SM, Yun KH, Cho JY, Kim CJ, Ahn HS, Nam CW, Yoon HJ, Park YH, Lee WS, Choi KH, Park TK, Yang JH, Choi SH, Gwon HC, Song YB, Hahn JY, Jeong DS, Lee JM. Intravascular Imaging-Guided PCI vs Coronary Artery Bypass Grafting for Left Main or 3-Vessel Disease. JACC Cardiovasc Interv. 2025 Sep 8;18(17):2077-2088. doi: 10.1016/j.jcin.2025.06.034. Epub 2025 Aug 27. PMID: 40864021.
2. Head SJ, Mack MJ, Holmes DR Jr, et al. Anatomy versus Physiology for Revascularization Decisions: The Left Main and Multivessel Disease Dilemma. J Am Coll Cardiol. 2020;75(12):1530-1542.
3. Stone GW, Sabik JF, Serruys PW, et al. CABG versus PCI for Left Main Coronary Artery Disease. N Engl J Med. 2019;381(20):1822-1832.