Highlights
- Veligrotug, an anti-IGF-1R antibody, has shown significant efficacy in reducing proptosis and diplopia in both active and chronic thyroid eye disease (TED) in phase 3 clinical trials (THRIVE, THRIVE-2).
- The regimen offers a shortened infusion protocol—five infusions at three-week intervals, each lasting 30 minutes—compared to teprotumumab, potentially improving patient convenience and adherence.
- Safety profile is manageable, with mild adverse events predominating and rates of hearing impairment similar to other IGF-1R inhibitors.
- Veligrotug has received Breakthrough Therapy designation from the FDA, expediting its review as an alternative to teprotumumab.
Clinical Background and Disease Burden
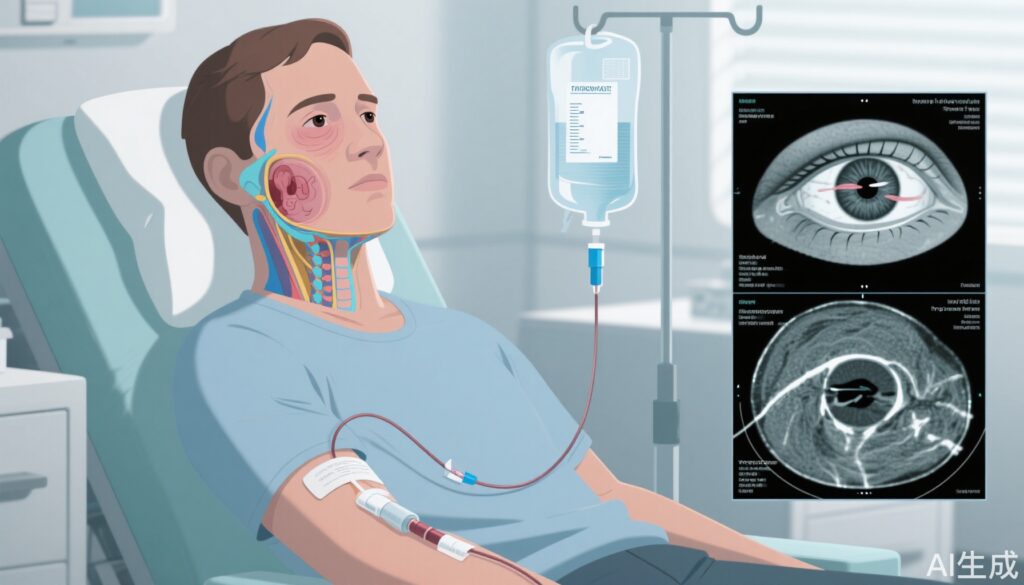
Thyroid eye disease (TED), also known as Graves’ orbitopathy, is a sight-threatening autoimmune disorder characterized by inflammation and remodeling of orbital tissues. The disease manifests with proptosis (eyeball protrusion), diplopia (double vision), periorbital edema, and, in severe cases, vision loss due to compressive optic neuropathy. Beyond physical morbidity, TED imposes a heavy psychosocial and quality-of-life burden, impacting self-image, emotional well-being, and daily functioning.
Current therapeutic options are limited. Teprotumumab, a monoclonal antibody targeting the insulin-like growth factor-1 receptor (IGF-1R), is the only FDA-approved therapy for TED, demonstrating substantial benefit in randomized trials but also notable adverse effects, including hearing loss and hyperglycemia. The need for alternative agents with improved convenience, safety, and efficacy remains pressing.
Research Methodology
The efficacy and safety of veligrotug, another anti-IGF-1R monoclonal antibody, were evaluated in two large phase 3, randomized, placebo-controlled trials: THRIVE and THRIVE-2.
THRIVE Trial (Active TED):
– Population: 113 adults (North America, Australia, Europe) with moderate-to-severe, active TED of ≤15 months’ duration and ≥3 mm proptosis.
– Intervention: Randomization to veligrotug (10 mg/kg IV, n=75) or placebo (n=38), 5 infusions at 3-week intervals.
– Baseline: Mean proptosis 23.2 mm, Clinical Activity Score (CAS) ~4.5–4.8, diplopia in ~68%.
– Endpoints: Proptosis responder rate (PRR, ≥2 mm reduction), change in CAS, diplopia resolution, safety.
THRIVE-2 Trial (Chronic TED):
– Population: 188 adults with moderate-to-severe, chronic TED (proptosis >2 mm above normal).
– Intervention: Randomization to veligrotug (n=125) or placebo (n=63), same regimen as THRIVE.
– Endpoints: PRR by Hertel and MRI/CT, diplopia response, CAS improvement, safety.
Key Findings
THRIVE (Active TED):
– At 15 weeks, 70% of veligrotug patients achieved ≥2 mm reduction in proptosis (Hertel), vs 5% with placebo (mean reduction: 2.9 mm vs 0.5 mm; P<0.0001).
– MRI/CT PRR: 69% for veligrotug vs 9% for placebo (2.9 mm vs 0.6 mm; P<0.0001).
– Mean CAS reduction: 3.4 (veligrotug) vs 1.7 (placebo; P<0.0001).
– Diplopia resolution: 54% (veligrotug) vs 12% (placebo; P<0.0001).
– Early response: Improvements observed as early as 3 weeks post-infusion.
– Durability: 70% of week-15 proptosis responders maintained response at week 52 (per press release).
THRIVE-2 (Chronic TED):
– At 15 weeks, 56% of veligrotug patients achieved ≥2 mm proptosis reduction (Hertel), vs 8% with placebo (mean: 2.9 mm vs 0.5 mm; P<0.0001).
– MRI/CT PRR: 48% (veligrotug) vs 3% (placebo; P<0.0001).
– Diplopia responder rate: 56% (veligrotug) vs 25% (placebo); complete resolution in 32% vs 14% (P=0.0152).
– CAS 0/1 achieved in 54% (veligrotug) vs 24% (placebo) in those with baseline CAS ≥3 (P=0.0060).
– Efficacy apparent within 3 weeks of first infusion.
Safety:
– Adverse events (AEs) were generally mild; most common were muscle spasms (36% veligrotug vs 6% placebo) and menstrual disorders (33% vs 10% among menstruating women).
– Hearing impairment: 13–16% (veligrotug) vs 3–11% (placebo), comparable to rates seen with teprotumumab (10–29% in studies).
– Serious AEs were infrequent and largely unrelated to treatment.
– Caution warranted in patients with preexisting hearing loss, hyperglycemia, or inflammatory bowel disease.
Mechanistic Insights
Veligrotug, like teprotumumab, targets IGF-1R. In TED, IGF-1R is overexpressed on orbital fibroblasts and immune cells, amplifying inflammatory signaling and tissue remodeling. Blockade of IGF-1R reduces autoantibody-mediated activation, thereby diminishing inflammation, tissue expansion, and fibrosis in the orbit. The similar efficacy profiles between veligrotug and teprotumumab support this mechanism.
Adverse hearing effects observed with IGF-1R inhibitors are hypothesized to involve disruption of cochlear hair cell function or inflammation; these are usually reversible but may be more severe in those with preexisting hearing loss.
Expert Commentary
Dr. Amy Patel Jain, lead author of THRIVE-2, emphasized the significance of demonstrating efficacy in both active and chronic TED, particularly for diplopia—a symptom with major quality-of-life implications. Dr. Mudumbai highlighted the need for vigilance regarding hearing effects and metabolic complications but noted that most adverse events are transient and manageable.
Controversies and Limitations
– The THRIVE trials were industry-sponsored, raising the need for independent confirmation.
– Long-term safety remains under study; hearing loss and hyperglycemia require further surveillance, especially in real-world populations with comorbidities.
– Generalizability to milder forms of TED or populations with significant comorbidities is not established.
– Head-to-head trials versus teprotumumab are lacking, though indirect comparisons suggest similar efficacy.
Conclusion
Veligrotug represents a substantial advance in the management of TED, offering a shorter, less burdensome infusion regimen and strong efficacy for both active and chronic disease. Its safety profile is comparable to existing IGF-1R inhibitors, with manageable risks. Pending full regulatory review and post-marketing surveillance, veligrotug may soon offer clinicians and patients a valuable new option, particularly for those who are intolerant of or relapse after teprotumumab.
References
1. Barnett MJL, Lam J, Jara-Tantoco MN, et al. Teprotumumab and sensorineural hearing loss: a propensity score-matched retrospective cohort study. Endocr Connect. 2025;14(7):e250293. doi:10.1530/EC-25-0293.
2. Abumohssin AG, Alshareef RA, Aljohani S, et al. Comparative efficacy and safety of rituximab, tocilizumab, and teprotumumab in Graves’ orbitopathy: a systematic review and meta-analysis. Eye (Lond). 2025;39(10):1901-1932. doi:10.1038/s41433-025-03845-8.
3. Ugradar S, Parunakian E, Malkhasyan E, et al. The Rate of Re-treatment in Patients Treated with Teprotumumab: A Multicenter Study of 119 Patients with 1 Year of Follow-up. Ophthalmology. 2025;132(1):92-97. doi:10.1016/j.ophtha.2024.07.018.