Highlight
• De-escalated adjuvant radiotherapy (30-36 Gy) combined with docetaxel significantly reduces chronic grade 3 or higher toxicities compared to standard adjuvant chemoradiotherapy (60 Gy plus cisplatin) in HPV-associated oropharyngeal squamous cell carcinoma.
• The study demonstrates a 3% versus 11% cumulative chronic high-grade toxicity rate favoring de-escalation, including lower PEG tube dependency.
• The trial supports the safety and tolerability of the de-escalated regimen in a well-defined intermediate-risk patient population.
• These findings encourage further clinical exploration of personalized radiation dosing strategies in HPV-related head and neck cancer.
Study Background and Disease Burden
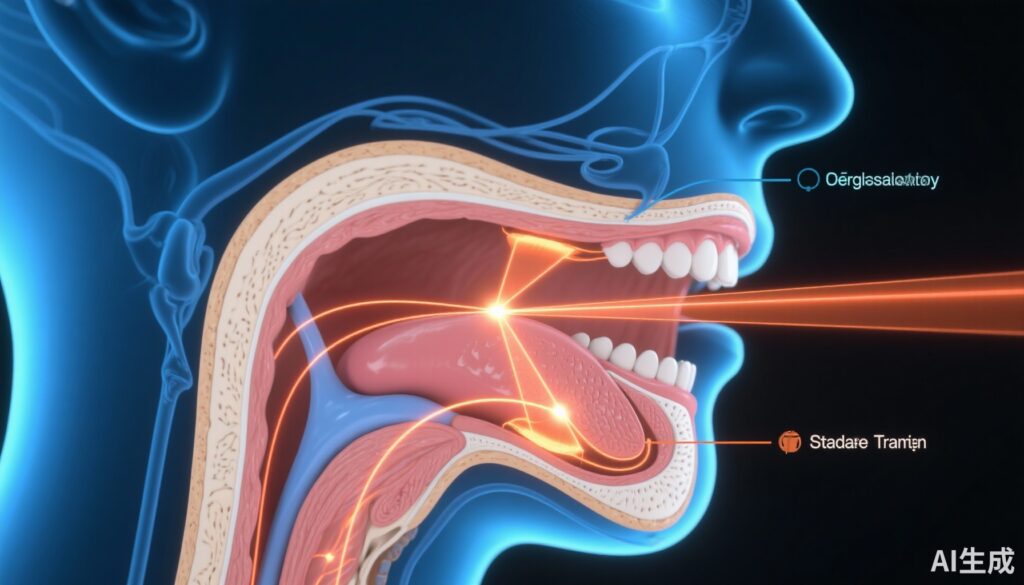
Human papillomavirus (HPV)-associated oropharyngeal squamous cell carcinoma (OPSCC) has emerged as a distinct clinical entity characterized by improved prognosis compared to HPV-negative disease. Standard management following surgical resection commonly includes adjuvant chemoradiotherapy with radiation doses of 60 to 66 Gy combined with cisplatin to reduce recurrence risk. While this approach achieves excellent oncologic control, patients experience significant treatment-related morbidities including dysphagia, mucositis, xerostomia, and long-term feeding tube dependence.
Given the generally favorable prognosis of HPV-positive OPSCC, reducing treatment-related toxicity without compromising effectiveness is a critical unmet need. De-escalated radiotherapy approaches have been proposed, aiming to minimize radiation-induced damage to normal tissues. However, rigorous evidence from randomized controlled trials comparing reduced-dose radiotherapy with standard care in this setting had been lacking.
Study Design
This was a phase 3, open-label, randomized controlled trial conducted at two US academic centers investigating de-escalated adjuvant radiotherapy in HPV-associated OPSCC. Eligible adults had pathological stage III–IV disease per AJCC 7th edition, demonstrated >70% p16 immunoreactivity, ECOG performance status 0 or 1, and at least one intermediate pathological risk factor after surgery. Stratification factors included extranodal extension and smoking status (<10 vs ≥10 pack-years).
Patients were randomized in a 2:1 ratio to receive either:
- De-escalated Radiotherapy (DART) Group: 30-36 Gy delivered in 1.5-1.8 Gy fractions twice daily over 2 weeks plus intravenous docetaxel 15 mg/m² on days 1 and 8.
- Standard of Care Group: 60 Gy in 2 Gy fractions once daily over 6 weeks plus weekly intravenous cisplatin 40 mg/m².
The primary endpoint was the cumulative incidence of chronic grade 3 or higher toxicities occurring between 3 and 24 months post-radiotherapy. Analysis focused on treated patients without missing endpoint data.
Key Findings
Between October 2016 and August 2020, 254 patients were screened and 228 enrolled. Of these, 194 proceeded to treatment and analysis (130 in DART, 64 standard care). Median age was approximately 59 years, predominantly male (89%) and White (95%). Median follow-up exceeded 3 years.
The primary outcome demonstrated a significant reduction in chronic severe toxicities with DART: 3% (4/125 patients) versus 11% (7/62 patients) in the standard group (p=0.042). Notably, the incidence of percutaneous endoscopic gastrostomy (PEG) dependence was lower, 2% versus 8% (p=0.039), marking an important quality-of-life metric.
Specific grade 3+ toxicities in the DART arm included dysphagia (2%), esophagitis (1%), and hearing impairment (1%). In contrast, the standard group experienced higher rates of dysphagia (8%), esophagitis (2%), fatigue (2%), pain (2%), and osteonecrosis of the jaw (2%).
While the study primarily assessed toxicity, outcomes related to oncological efficacy—though not detailed here—were presumably comparable or previously established given the rationale for dose de-escalation in HPV-positive intermediate-risk patients.
Expert Commentary
This landmark trial provides compelling evidence supporting the feasibility and safety of de-escalated adjuvant chemoradiotherapy in HPV-associated oropharyngeal cancer with intermediate risk features. The significant toxicity reduction observed, including lower PEG tube reliance, addresses the profound morbidity burden associated with standard high-dose regimens.
By leveraging the tumor’s favorable biology and sensitivity to treatment, this approach may represent an important step toward personalized, risk-adapted therapies that preserve efficacy while enhancing patient quality of life. The study’s randomized design and robust stratification strengthen the validity of findings.
Limitations include the open-label design and a predominantly White population, which may affect generalizability. Long-term oncologic outcomes such as progression-free and overall survival data are awaited to further validate this de-escalation strategy. Furthermore, incorporation of patient-reported outcomes and functional assessments would enrich understanding of the clinical impact.
Current clinical guidelines acknowledge the promise of treatment de-intensification in select HPV-positive patients, but this trial marks a pivotal evidence base enabling more confident integration into practice pending confirmatory studies.
Conclusion
The MC1675 phase 3 trial rigorously demonstrates that de-escalated adjuvant radiotherapy combined with docetaxel markedly reduces chronic grade 3 or higher toxicities compared to standard chemoradiotherapy in intermediate-risk HPV-associated oropharyngeal squamous cell carcinoma. This strategy markedly lowers debilitating side effects such as dysphagia and PEG dependency, potentially improving survivorship quality without sacrificing oncologic safety.
These findings support further clinical investigation and consideration of the DART regimen in appropriate patient populations. Ultimately, such personalized therapeutic modifications may transform the management paradigm by optimizing the balance between efficacy and long-term treatment-related morbidity in this distinct cancer subgroup.
References
- Ma D, Price K, Moore E, et al. De-escalated adjuvant radiotherapy versus standard adjuvant treatment for human papillomavirus-associated oropharyngeal squamous cell carcinoma (MC1675): a phase 3, open-label, randomised controlled trial. Lancet Oncol. 2025 Sep;26(9):1227-1239. doi: 10.1016/S1470-2045(25)00324-9. PMID: 40907518.
- Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24-35. doi:10.1056/NEJMoa0912217.
- Yom SS, Torres-Saavedra P. De-Intensification for HPV-Associated Oropharynx Cancer: Trials and Tribulations. Int J Radiat Oncol Biol Phys. 2021;110(5):1244-1248. doi:10.1016/j.ijrobp.2021.02.022.