Highlight
– Lanifibranor reduces intrahepatic triglyceride content by approximately 50% over 24 weeks in patients with type 2 diabetes and metabolic dysfunction-associated steatotic liver disease (MASLD).
– Treatment significantly improves insulin resistance at hepatic, muscle, and adipose tissue levels by enhancing glucose metabolism.
– Cardiometabolic risk factors, including HbA1c, HDL cholesterol, and adiponectin, showed marked improvement.
– Lanifibranor demonstrated a favorable safety profile with only mild adverse effects and minimal weight gain.
Study Background and Disease Burden
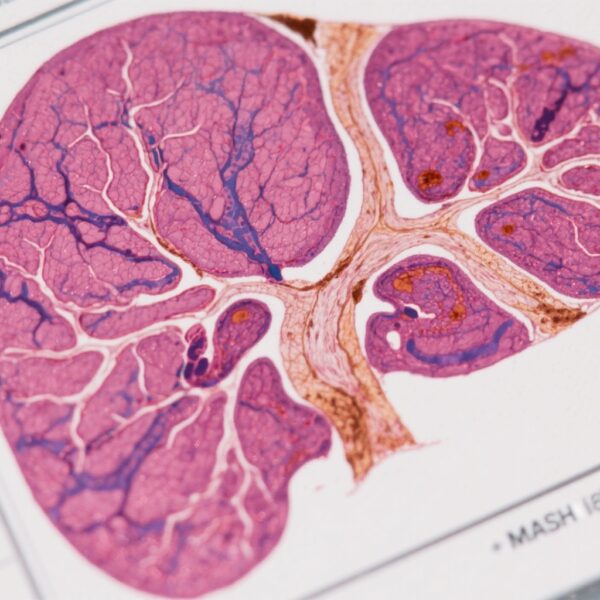
Metabolic dysfunction-associated steatotic liver disease (MASLD) is increasingly common among patients with type 2 diabetes (T2D), presenting a substantial burden due to its association with insulin resistance, hepatic steatosis, progression to steatohepatitis, fibrosis, and increased cardiovascular risk. Currently, no FDA-approved therapies specifically target MASLD or the related metabolic impairments. Peroxisome proliferator-activated receptors (PPARs) are nuclear receptors essential in regulating lipid and glucose metabolism. Lanifibranor is a novel pan-PPAR agonist with the potential to address multiple pathophysiological aspects of MASLD.
Study Design
This was a single-center, randomized, placebo-controlled phase II trial that enrolled 38 patients with T2D and MASLD. Participants were randomized in a 1:1 ratio to receive either lanifibranor 800 mg daily or placebo for 24 weeks. The primary endpoint was the change in intrahepatic triglyceride (IHTG) content assessed by proton magnetic resonance spectroscopy (1H-MRS). Key secondary endpoints included assessing insulin sensitivity across liver, muscle, and adipose tissue using the euglycemic hyperinsulinemic clamp technique—the gold standard for insulin resistance evaluation. Other secondary outcomes comprised changes in cardiometabolic parameters such as HbA1c, lipid profile, and adiponectin levels.
Key Findings
Lanifibranor treatment resulted in a significant reduction in IHTG levels compared to placebo. In the full analysis set (FAS), IHTG content declined by 44% with lanifibranor versus 12% with placebo, corresponding to a least squares mean difference of -31% (95% CI, -51 to -12%; p <0.01). In study completers, the reduction was even more pronounced, at 50% versus 16% (p <0.01). A considerably higher proportion of patients treated with lanifibranor achieved clinically meaningful endpoints—65% versus 22% in the FAS and 79% versus 29% in completers attained ≥30% reduction in IHTG. Additionally, steatosis resolution occurred in 25% of lanifibranor patients versus none in the placebo arm (p <0.05).
| FAS, N = 38 | Completers, n = 28 | |||||||
|---|---|---|---|---|---|---|---|---|
| Adjusted LS mean [95% CI] | Adjusted LS mean difference [95% CI] | p value | Adjusted LS mean [95% CI] | Adjusted LS mean difference [95% CI] | p value | |||
| Lanifibranor n = 20 | Placebo n = 18 | Lanifibranor vs. placebo | Lanifibranor n = 14 |
Placebo n = 14 |
Lanifibranor vs. placebo | |||
| Primary endpoint | ||||||||
| Absolute change from baseline (%) in IHTG | -8.7 [-11.3; -6.0] | -3.0 [-5.9; -0.2] | -5.6 [-9.6; -1.7] | 0.007 [1] | -10.8 [-13.6; -8.1] | -4.0 [-6.7; -1.2] | -6.9 [-10.8; -2.9] | 0.001 [1] |
| Relative change from baseline (%) in IHTG | -44 [-57; -31] | -12 [-26; 2] | -31 [-51; -12] | 0.002 [1] | -50 [-64; -36] | -16 [-30; -3] | -33 [-53; -14] | 0.002 [1] |
| Secondary continuous endpoints | ||||||||
| Relative change from baseline in | ||||||||
| Fasting hepatic glucose production (%) | -8 [-13; -4] | 4 [-1; 9] | -13 [-20; -6] | <0.001 [1] | -12 [-19; -5]∗ | 4 [-2; 11] | -16 [-26; -7] | 0.001 [1] |
| Hepatic IR index (%) | -26 [-37; -14] | -7 [-19; 4] | -18 [-34; -2] | 0.04 [1] | -39 [-54; -24]∗ | -10 [-24; 3] | -29 [-49; -9] | 0.007 [1] |
| Insulin-stimulated muscle glucose disposal (%) | 30 [13; 46] | 0 [-17; 18] | 29 [5; 54] | 0.02 [1] | 45 [23; 67]∗ | 0 [-22; 23] | 45 [12; 77] | 0.009 [1] |
| Absolute change from baseline in: | ||||||||
| Fasting plasma insulin (μU/ml) | -3.1 [-5.5; -0.8] | -0.0 [-2.5; 2.5] | -3.1 [-6.5; 0.3] | 0.07 [1] | -4.3 [-7.5; -1.2] | -0.1 [-3.3; 3.1] | -4.2 [-8.7; 0.3] | 0.07 [1] |
| Fasting plasma glucose (mg/dl) | -17.2 [-27.4; -7.0] | 2.4 [-8.4; 13.2] | -19.6 [-34.5; -4.7] | 0.01 [2] | -19.4 [-31.3; -7.4] | -3.5 [-15.5; 8.4] | -15.8 [-32.8; 1.1] | 0.07 [2] |
| HOMA-IR | -1.6 [-2.5; -0.7] | -0.1 [-1.1; 0.8] | -1.5 [-2.8; -0.2] | 0.03 [1] | -2.4 [-3.7; -1.1] | -0.3 [-1.5; 0.9] | -2.1 [-3.8; -0.3] | 0.02 [1] |
| Adipo-IR | -2.7 [-4.3; -1.2] | -0.7 [-2.4; 0.9] | -2.0 [-4.2; 0.3] | 0.08 [1] | -3.9 [-5.9; -1.9] | -0.9 [-2.9; 1.1] | -3.0 [-5.8; -0.20] | 0.04 [1] |
| HbA1c (%) | -0.7 [-1.0; -0.5] | -0.1 [-0.3; 0.2] | -0.6 [-1.0; -0.5] | <0.001 [2] | -0.9 [-1.2; -0.7] | -0.2 [-0.5; 0.0] | -0.7 [-1.1; -0.4] | <0.001 [2] |
| HDL-C (mg/dl) | 7.6 [4.4; 10.7] | 0.9 [-2.4; 4.3] | 6.6 [2.0; 11.3] | 0.006 [2] | 6.3 [2.6; 10.1] | -0.3 [-4.0; 3.5] | 6.6 [1.3; 11.9] | 0.016 [2] |
| Fold change from baseline in | ||||||||
| Adiponectin | 2.4 [2.0; 2.7] | 1.0 [0.6; 1.4] | 1.4 [0.9; 1.9] | <0.001 [2] | 2.7 [2.3; 3.1] | 1.0 [0.6; 1.4] | 1.7 [1.2; 2.4] | <0.001 [2] |
| Secondary categorical endpoints | % [95% CI] | p value | % [95% CI] | p value | ||||
| Lanifibranor | Placebo | Lanifibranor vs. placebo | Lanifibranor | Placebo | Lanifibranor vs. placebo | |||
| ≥30% reduction in IHTG | 65 [41; 85] | 22 [6; 48] | 0.008 [3] | 79 [49; 95] | 29 [8; 58] | 0.008 [3] | ||
| Steatosis resolution (IHTG ≤5.5%) | 25 [9; 49] | 0 [0; 19] | 0.048 [4] | 21 [5; 51] | 0 [0; 23] | 0.048 [4] | ||
Importantly, lanifibranor led to significant improvements in insulin resistance across multiple tissues. Fasting endogenous glucose production, primarily hepatic, was reduced, indicating enhanced hepatic insulin sensitivity. Insulin-stimulated glucose disposal rates (Rd), reflecting skeletal muscle insulin sensitivity, were also markedly improved. Adipose tissue insulin sensitivity was restored, as evidenced by metabolic parameter shifts and a 2.4-fold increase in adiponectin, an adipocyte-derived hormone that enhances insulin sensitivity and anti-inflammatory responses (all p <0.001).

Secondary cardiometabolic outcomes showed meaningful improvements: fasting glucose, fasting insulin, homeostatic model assessment for insulin resistance (HOMA-IR), HbA1c, and high-density lipoprotein cholesterol (HDL-C) all improved significantly in the lanifibranor group compared to placebo (p <0.001). Body weight increased modestly by +2.7% in lanifibranor-treated individuals, a side effect warranting further monitoring.
Adverse events were predominantly mild, with gastrointestinal symptoms and minor hemoglobin decrease reported without significant clinical consequences. Drug-related treatment-emergent adverse events leading to study discontinuation were balanced between groups, supporting an acceptable safety profile over 24 weeks.
Expert Commentary
The study by Barb et al. provides critical insights into the mechanistic and clinical benefits of lanifibranor in a cohort with dual burdens of T2D and MASLD. Unlike previous investigations focusing predominantly on hepatic outcomes, this trial uniquely evaluated insulin sensitivity at the level of liver, muscle, and adipose tissue using the hyperinsulinemic clamp technique. The comprehensive improvement across these metabolically important tissues supports the concept of pan-PPAR activation as a systemic therapeutic strategy.
The observed adiponectin elevation corroborates previous findings linking PPAR activation to enhanced adipocyte function and systemic insulin sensitization. The modest weight gain, while notable, may reflect improved adipose tissue capacity for lipid storage rather than adverse metabolic deterioration, though longer-term studies are needed to delineate its clinical relevance fully.
Limitations include the small sample size and single-center design, which may affect generalizability. Furthermore, the 24-week duration limits assessment of longer-term efficacy and safety, particularly regarding fibrosis progression. Ongoing phase III studies will be pivotal in confirming these preliminary findings and establishing clinical guidelines.
Conclusion
Lanifibranor emerges as a promising therapeutic agent targeting fundamental metabolic disturbances in patients with T2D and MASLD. This phase II trial demonstrates its capacity to significantly reduce hepatic steatosis while improving insulin sensitivity in liver, muscle, and adipose tissue, effectively addressing the multifaceted pathophysiology of MASLD. Improvements in key cardiometabolic risk factors further enhance its clinical appeal.
The results provide robust proof-of-concept evidence that targeting intrinsic metabolic mechanisms—insulin resistance, lipotoxicity, hyperglycemia—can restore cardiometabolic health in MASLD. Lanifibranor thus offers a compelling treatment approach either as monotherapy or combined with lifestyle interventions such as weight loss. Further large-scale, long-term studies are warranted to confirm these benefits and elucidate effects on fibrosis and clinical outcomes.
References
- Barb D, Kalavalapalli S, Godinez Leiva E, Bril F, Huot-Marchand P, Dzen L, Rosenberg JT, Junien JL, Broqua P, Rocha AO, Lomonaco R, Abitbol JL, Cooreman MP, Cusi K. Pan-PPAR agonist lanifibranor improves insulin resistance and hepatic steatosis in patients with T2D and MASLD. J Hepatol. 2025 Jun;82(6):979-991. doi: 10.1016/j.jhep.2024.12.045 IF: 33.0 Q1 . Epub 2025 Jan 15. PMID: 39824443 IF: 33.0 Q1 .
- Ratziu V, et al. Targeting metabolic pathways in NAFLD: the role of PPAR agonists. Hepatology. 2022;75(6):1529-1543.
- Bril F, Cusi K. Management of nonalcoholic fatty liver disease in patients with type 2 diabetes: a call to action. Diabetes Care. 2017 Sep;40(9):1232-1242.