Introduction: The Silent Threat Beyond Cholesterol
For decades, the triumvirate of high cholesterol, hypertension, and diabetes has been recognized as the primary driver behind atherosclerosis — the thickening and stiffening of arteries that leads to heart attacks and strokes. These well-known “villains” damage the inner walls of blood vessels, eventually causing life-threatening cardiovascular events.
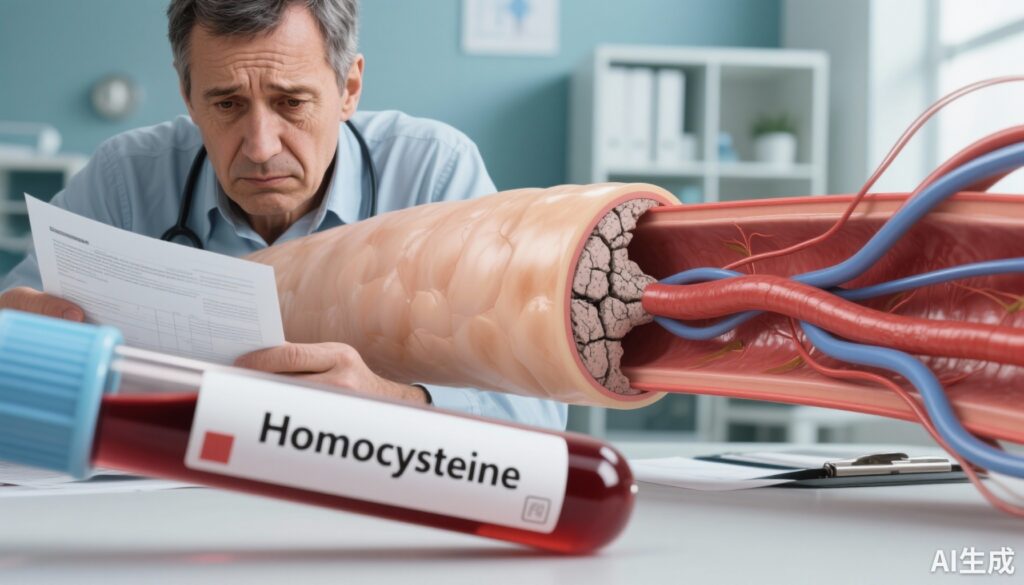
Yet lurking in our bloodstream is a less familiar yet no less dangerous adversary: homocysteine (Hcy). Unlike cholesterol, homocysteine has flown under the radar, overshadowed by traditional lipid markers. However, emerging evidence indicates that elevated homocysteine levels can independently accelerate arterial aging and dysfunction.
A recent landmark study published in the internationally respected journal Acta Biomaterialia sheds light on how high homocysteine levels cause the aorta—the body’s main artery—to stiffen and lose elasticity without the presence of high cholesterol. This finding could shift the paradigm of cardiovascular prevention and treatment.
The Overlooked Independent Killer: Homocysteine
Atherosclerosis has long been viewed primarily as a lipid-driven disease. However, clinicians observe plenty of patients with normal cholesterol who still suffer cardiovascular events. This conundrum prompted researchers to ask: Could there be other independent risk factors beyond elevated blood lipids?
The answer is yes. Elevated homocysteine, medically termed hyperhomocysteinemia (HHcy), is one such factor.
The link between homocysteine and vascular disease was first established over 50 years ago. In 1969, American pathologist Kilmer McCully discovered that children with genetic homocystinuria—a condition causing excessive homocysteine—exhibited severe early-onset arterial disease. This pivotal observation connected homocysteine to vascular damage.
Since then, epidemiological data have reinforced this connection:
– For every 2.5 μmol/L increase in blood homocysteine, cardiovascular disease risk rises by approximately 10%.
– About 40% of patients experiencing early coronary artery disease or peripheral vascular disease have elevated homocysteine.
– Homocysteine not only independently increases atherosclerosis risk but also predicts cardiovascular mortality.
Until recently, how homocysteine mechanically alters blood vessels remained mysterious. The latest animal study now reveals direct biomechanical effects.
New Insights: How Homocysteine Weakens and Hardens Arteries
Researchers conducted a controlled experiment using rabbits, dividing them into groups receiving different diets and treatments:
– Standard Diet (SD): Control group with normal nutrition.
– Vitamin-Choline Deficient Diet (VCDD): Lacking folate, vitamins B6, B12, and choline.
– High Cholesterol Diet (HCD): Promotes arterial plaque formation.
– Dual Deficiency + High Cholesterol (DD): Combination of nutrient deficiency and high cholesterol.
– Some rabbits additionally received injections of homocysteine to elevate blood levels further.
Findings were striking:
– Rabbits on the VCDD exhibited a doubling of blood homocysteine.
– Those given VCDD plus homocysteine injections had levels elevated by 3.5 times.
– Critically, rabbits with elevated homocysteine but normal cholesterol showed significant stiffening of the aorta.
Mechanical testing simulating physiological blood vessel stress showed that vitamin and choline deficiency — leading to high homocysteine — caused the aorta to become stiffer in both lengthwise and circular directions. Additional homocysteine injections amplified these effects, manifesting as heightened stress responses and energy dissipation indicative of decreased vascular elasticity.
Conversely, the high cholesterol group developed marked atherosclerotic plaques but their arteries paradoxically became softer overall.
This study highlights a fundamental distinction:
– Cholesterol drives plaque formation obstructing arteries.
– Homocysteine predominantly drives vascular stiffening by altering vessel wall structure and mechanics.
Why Does Homocysteine Harden Blood Vessels?
Biochemically, homocysteine is an intermediate metabolite in methionine metabolism. Its removal depends on three critical pathways:
1. Remethylation Pathway: Folate and vitamin B12 are required to convert homocysteine back to methionine.
2. Transsulfuration Pathway: Vitamin B6 enables conversion into harmless cysteine.
3. Betaine Pathway: Betaine, derived from choline, serves as a methyl donor to assist homocysteine metabolism.
Deficiencies in folate, vitamins B6 and B12, or choline disrupt these pathways, causing homocysteine accumulation in blood.
Excess homocysteine exerts multiple harmful effects:
– Stimulates excessive growth of vascular smooth muscle cells.
– Encourages collagen overproduction while inhibiting elastin synthesis, decreasing arterial elasticity.
– Activates inflammatory and oxidative stress processes that damage endothelial function.
– Interferes with collagen cross-linking, leading to abnormal connective tissue growth resembling a “vascular Marfan syndrome.”
Over time, these processes stiffen the vessel wall, make it brittle, and impair its elasticity — hallmarks of atherosclerosis progression.
Is Your Homocysteine Level in Check?
Normal blood homocysteine is generally accepted to be below 15 μmol/L. However, in individuals with hypertension, diabetes, or other cardiovascular risks, levels above 10 μmol/L warrant attention.
In China, for example, over 20% of adults show elevated homocysteine, especially older men and those with unbalanced diets.
Even more concerning, individuals with “H-type hypertension” — characterized by both high blood pressure and elevated homocysteine — have more than 10 times the stroke risk compared to those with normal homocysteine levels.
Strategies to Lower Homocysteine Levels Effectively
The good news is that elevated homocysteine is preventable and manageable through nutritional and lifestyle measures:
1. Supplement Methyl Donors: Folate and Betaine
– Daily folate (0.8 mg) supplementation reduces homocysteine significantly.
– Folate-rich foods include leafy greens (spinach, broccoli), liver, and legumes.
– Betaine (also known as trimethylglycine) is found in beets, whole grains, spinach, and shellfish; typical supplements range 500–2000 mg/day taken with meals to minimize gastrointestinal side effects.
2. Complete the B-Vitamin Triad
– Vitamin B6 (1.7 mg/day for men, 1.5 mg/day for women): Sources are chicken, fish, bananas, nuts, and potatoes.
– Vitamin B12, critical but often deficient in older adults, vegetarians, and metformin users: Found in red meat, deep-sea fish, dairy, and shellfish.
– Combination supplements containing folate, B6, B12, and betaine yield synergistic benefits.
3. Consider Genetic Variations
– Around 5–15% of people carry the MTHFR C677T gene variant that impairs folate metabolism.
– These individuals may not efficiently convert standard folic acid to its active form, 5-methyltetrahydrofolate (5-MTHF).
– Genetic testing helps identify who would benefit from direct 5-MTHF supplementation and vitamin B2 intake to optimize enzyme function.
4. Maintain a Healthy Lifestyle
– Though genetics and nutrition dominate homocysteine metabolism, high-fat/high-sugar diets, sedentary habits, smoking, excessive alcohol, and aging increase levels.
– Balanced diet, regular exercise, smoking cessation, and moderated alcohol intake protect cardiovascular health holistically.
Case Scenario: John’s Hidden Risk
John, a 55-year-old office worker with controlled hypertension, recently suffered a mild stroke. Despite normal cholesterol and glucose levels, his homocysteine was 14 μmol/L, above the safe threshold. Genetic testing revealed an MTHFR variant. After starting tailored supplementation with active folate, B vitamins, and betaine, plus lifestyle improvements, his homocysteine dropped to safe levels, reducing future cardiovascular risks.
John’s case exemplifies the silent danger of homocysteine and the benefits of targeted screening and intervention.
Conclusion: Rethinking Cardiovascular Risk Beyond Lipids
Atherosclerosis is a complex, progressive condition. While cholesterol, blood pressure, and blood sugar remain crucial markers, homocysteine emerges as a stealthy “vascular assassin” that independently stiffens arteries and accelerates disease.
The recent biomechanical findings elucidate how elevated homocysteine uniquely alters vessel wall structure and function, leading to early arterial hardening that precedes plaque buildup.
Regular screening for homocysteine, especially in high-risk groups, combined with personalized vitamin supplementation and healthy lifestyle choices, can significantly mitigate cardiovascular risk.
Protecting vascular health demands expanding our focus beyond “lowering lipids” to also “detoxifying” metabolism by addressing homocysteine—an overlooked yet modifiable threat to arterial integrity.
References
– Homocysteine leads to aortic stiffening in a rabbit model of atherosclerosis, Acta Biomaterialia, Volume 201, 2025, Pages 412-428.
– McCully KS. Vascular pathology of homocysteinemia: implications for the pathogenesis of arteriosclerosis. Am J Pathol. 1969;56(1):111-128.
– Wang X, Qin X, Demirtas H, et al. Efficacy of folic acid supplementation in stroke prevention: a meta-analysis. Lancet. 2007;369(9576):1876-1882.
– Refsum H, Ueland PM, Nygård O, Vollset SE. Homocysteine and cardiovascular disease. Annu Rev Med. 1998;49:31-62.
– Stanger O, Herrmann W, Pietrzik K, et al. Clinical use and rational management of homocysteine, folic acid, and B-vitamins in cardiovascular and thrombotic diseases. Z Kardiol. 2004;93(4):439-453.
[Note: Consult healthcare providers before starting any supplements or treatments.]