Highlight
- Rizedisben, a novel myelin-binding blue light fluorophore, effectively enhances intraoperative visualization of nerve structures in minimally invasive prostate surgery.
- Phase 1 open-label dose escalation in 38 patients determined 3.0 mg/kg as the optimal dose for sustained nerve fluorescence with minimal adverse effects.
- Sustained fluorescence of the obturator nerve was achieved in all patients at the optimal dose, with 89% visualization of prostate neurovascular bundles, crucial for nerve-sparing surgery.
- Rizedisben demonstrated a favorable safety profile, paving the way for phase 2 studies exploring broader surgical indications.
Study Background and Disease Burden
Fluorescence-guided surgery has revolutionized the intraoperative identification of critical anatomical structures, enhancing surgical precision and improving outcomes. Nerve preservation during radical prostatectomy is paramount to maintaining postoperative sexual and urinary function. However, intraoperative identification of nerves such as the obturator nerve and neurovascular bundles remains challenging due to their intricate anatomy and variable intra-individual presentation.
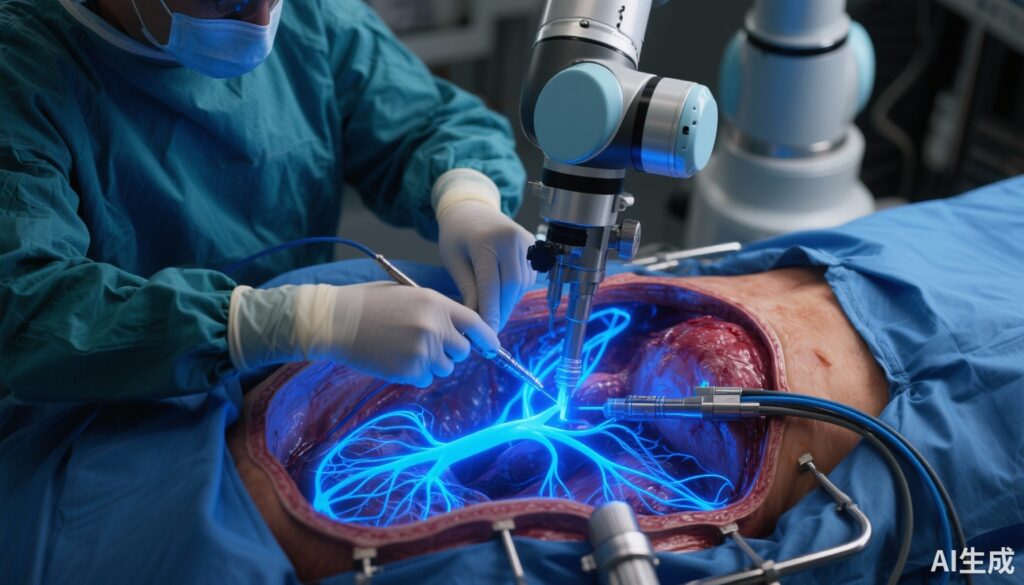
Rizedisben is a novel fluorophore that selectively binds myelin and fluoresces under blue light (370-425 nm), potentially allowing real-time visualization of nerve structures during surgery. Unlike standard white light illumination, this fluorescence-guided approach may reduce inadvertent nerve injury and improve patient quality of life postoperatively.
Given the unmet need for enhanced nerve visualization during robot-assisted laparoscopic radical prostatectomy (RALP), this study aimed to explore the safety and optimal dosing of rizedisben to achieve sustained intraoperative nerve fluorescence suitable for clinical utility.
Study Design
This was a single-arm, open-label, phase 1 clinical trial conducted at an urban academic cancer center in New York City between January 2023 and October 2024. The study population included adult patients (≥18 years) diagnosed with prostate cancer and scheduled for RALP. Key exclusion criteria comprised prior pelvic surgery or radiation, known central or peripheral nervous system disease, use of neurotoxic medications, recent exposure to phototoxic drugs, and significant renal or hepatic dysfunction, ensuring patient safety and minimizing confounding variables.
Using a dose escalation framework, rizedisben was administered intravenously intraoperatively 30 minutes before the anticipated visualization of the obturator nerve — the study’s reference nerve for fluorescence intensity. Doses ranged from 0.25 mg/kg to 3.0 mg/kg. Safety was continuously monitored, with dose escalation contingent on absence of dose-limiting toxicities.
The main outcomes were safety, assessed through 45 postoperative days, and fluorescence efficacy, measured via subjective intraoperative scoring complemented by post hoc objective image analysis. The clinically effective dose was defined stringently as that capable of producing sustained moderate or better fluorescence of the obturator nerve in ≥3 of 5 patients in two consecutive cohorts, with <20% incidence of grade 2 or higher toxicity. At the selected dose, additional fluorescence assessments of the prostate neurovascular bundles were performed to evaluate wider applicability.
Key Findings
Thirty-eight patients completed the trial, with a median age of 61.5 years (IQR 57.8-66.3). Dose escalation commenced at 0.25 mg/kg and progressed to 3.0 mg/kg. Safety analysis revealed only one grade 2 rash potentially attributable to rizedisben, reflecting a low adverse event profile suitable for further clinical development.
Critically, at the 3.0 mg/kg dose level, all patients (100%) demonstrated sustained fluorescence of the obturator nerve lasting 90 minutes or longer. This fluorescence was rated as moderate or better by subjective intraoperative assessment and confirmed by objective imaging metrics.
In addition to the obturator nerve, prostate neurovascular bundles exhibited fluorescence in 8 of 9 patients (89%) assessed at the 3.0 mg/kg dose. This finding is important for nerve-sparing prostatectomy techniques, as visual recognition of these bundles guides surgeons in avoiding injury.
The study provided clear dose-response data indicating that lower doses failed to achieve sustained fluorescence, while 3.0 mg/kg met the safety and efficacy criteria. Postoperative monitoring over 45 days did not reveal any severe toxicities, and no patients experienced grade 3 or higher adverse events related to the fluorophore.
Expert Commentary
The application of rizedisben as a fluorescence marker represents a significant advance in fluorescence-guided surgical techniques. By binding selectively to myelin and fluorescing within the blue light spectrum, rizedisben enables high-contrast visualization of neural tissue beyond what is achievable with traditional methods.
This trial’s design was exemplary in its methodical dose escalation, clearly defining efficacy thresholds and safety endpoints that align with clinical needs. Such rigorous criteria enhance the reliability of dose selection, providing robust evidence for the 3.0 mg/kg dose as the optimal balance between fluorescence intensity and tolerability.
While preliminary, these results are promising within the context of nerve-sparing prostatectomy, an area critically dependent on precise nerve identification to minimize postoperative dysfunction. The ability to visualize neurovascular bundles with high fidelity in nearly 90% of patients suggests substantial potential for rizedisben to improve functional outcomes.
Limitations of the study include its small sample size and single-arm design, which preclude direct comparison against standard care or other fluorophores. Additionally, long-term functional outcomes such as continence and sexual function were not evaluated, which will be essential in subsequent trials.
Further mechanistic studies may explore rizedisben’s specificity, kinetics, and potential off-target fluorescence. Additional investigations in diverse surgical fields and more extensive patient cohorts will solidify its clinical utility.
Conclusion
This phase 1 nonrandomized clinical trial demonstrates that rizedisben at 3.0 mg/kg intravenously delivers safe, sustained, and clinically meaningful fluorescence of nerve structures during robot-assisted laparoscopic radical prostatectomy. The enhanced visualization of both obturator nerves and neurovascular bundles lays the foundation for nerve-sparing approaches with potentially improved postoperative functional preservation.
Given the favorable safety profile and effective fluorescence achieved, these findings justify advancement to phase 2 studies that will investigate efficacy endpoints, broader surgical indications, and impact on patient-centered functional outcomes. Integrating rizedisben-guided fluorescence into minimally invasive surgery has the potential to redefine intraoperative anatomy identification and ultimately improve surgical precision and patient quality of life.
References
Gold SA, Pere MM, Assel M, Doudt AD, Durdin TD, Silagy AW, Dean LW, Recabal P, Levine E, Burke A, Ragupathi G, Marzabadi MR, Yao ZK, Yang G, Yang G, Ouerfelli O, McCarter M, Chen X, Tzatha E, Coleman JA, Goh AC, Smith RC, Ehdaie B, Vickers AJ, Scardino PT, Eastham JA, Laudone VP, Donahue TF. Rizedisben in Minimally Invasive Surgery: A Nonrandomized Clinical Trial. JAMA Surg. 2025 Aug 1;160(8):875-883. doi: 10.1001/jamasurg.2025.1987. PMID: 40601345; PMCID: PMC12224043.
Additional reviews on fluorescence-guided surgery and nerve visualization technologies may be found in:
– Peter M. Black et al., “Fluorescence-Guided Neurosurgery: Innovations and Patient Outcomes,” Neurosurgery. 2022 April; 90(4): 579-586.
– Smith R.C. et al., “Advances in Nerve Imaging and Surgical Navigation in Urology,” Urol Clin North Am. 2023;50(1):25-40.