Highlight
– Kidney tubular injury and dysfunction biomarkers, including IGFBP-7, KIM-1, MCP-1, and CCL-14, independently predict death and heart failure readmission in acute heart failure.
– These tubular biomarkers provide prognostic information beyond traditional kidney glomerular markers and cardiac biomarkers.
– IGFBP-7 specifically correlates with risk of death, whereas MCP-1 and CCL-14 associate with heart failure readmission.
– This study supports inclusion of tubular health assessment for risk stratification in acute heart failure management.
Study Background and Disease Burden
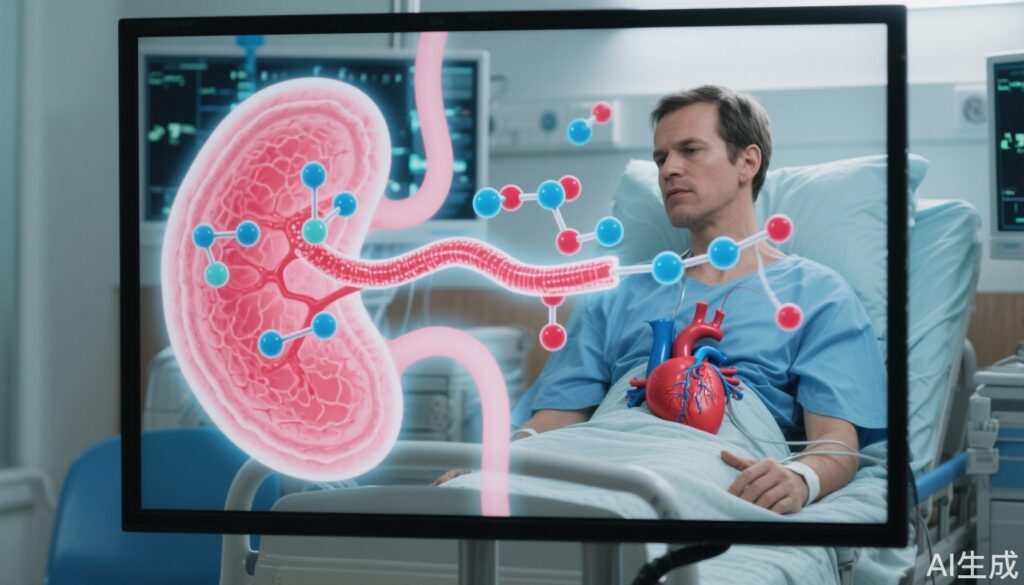
Acute heart failure (HF) is a common and serious clinical syndrome leading to substantial morbidity and mortality worldwide. Patients hospitalized with acute HF face high risks of death and rehospitalization. Kidney dysfunction, typically assessed by glomerular filtration rate (GFR), is established as an important prognostic factor in acute HF, indicating the complex cardio-renal interplay. However, kidney dysfunction is multifaceted and may involve glomerular damage as well as tubular injury and dysfunction.
Recent advances in biomarker discovery highlight that markers reflecting kidney tubular health can provide incremental clinical insights beyond traditional kidney function tests. Tubular biomarkers can detect subtle kidney injury and inflammatory processes that glomerular markers might miss. Determining whether these tubular biomarkers can predict clinical outcomes such as death and heart failure readmission could guide risk stratification, monitoring, and targeted therapies in acute HF.
Study Design
This investigation utilized data from AKINESIS (Acute Kidney Injury Neutrophil Gelatinase-Associated Lipocalin Evaluation of Symptomatic Heart Failure Study), a case-control cohort study enrolling 436 patients hospitalized with acute HF. Among them, 218 patients experienced acute kidney injury (AKI) at admission, matched with 218 patients without AKI to balance confounding.
Fourteen urine biomarkers representing kidney tubular damage and dysfunction were measured at hospital admission. The biomarkers included insulin-like growth factor binding protein-7 (IGFBP-7), kidney injury molecule-1 (KIM-1), monocyte chemoattractant protein-1 (MCP-1), tissue inhibitor of metalloproteinases-2 (TIMP-2), and C-C motif chemokine ligand-14 (CCL-14), among others.
The primary outcomes assessed were the composite of death or heart failure readmission, death alone, and heart failure readmission alone over 12 months. Multivariable Cox proportional hazards models adjusted for clinical confounders, kidney glomerular function (estimated glomerular filtration rate, eGFR), and cardiac biomarkers were used to evaluate associations.
Key Findings
The cohort had a mean age of 71 ± 12 years and included 64% men, with a mean eGFR of 55 ± 23 mL/min/1.73 m² at admission. Over one year, 156 patients experienced death or HF readmission, 87 died, and 92 had HF readmissions.
Significant associations were identified between tubular biomarkers and outcomes:
– Each twofold increase in IGFBP-7 was associated with a 36% higher risk of death or HF readmission (HR 1.36; 95% CI, 1.13–1.64).
– The IGFBP-7*TIMP-2 product was also linked to increased risk (HR 1.08; 95% CI, 1.01–1.14).
– KIM-1 levels correlated with a 12% higher risk (HR 1.12; 95% CI, 1.02–1.24).
– MCP-1 levels were associated with an 18% increased risk (HR 1.18; 95% CI, 1.03–1.34).
When analyzed by specific outcomes:
– IGFBP-7 predicted risk of death alone.
– MCP-1 and CCL-14 were significantly associated with HF readmission alone.
Importantly, these associations persisted after adjusting for traditional kidney function (eGFR) and established cardiac biomarkers, showing that tubular biomarkers provide unique prognostic information.
Expert Commentary
Dr. Nilay Wettersten and colleagues provide compelling evidence that kidney tubular injury markers add prognostic value in acute HF beyond conventional renal and cardiac risk indicators. These findings align with growing recognition that tubular health plays a central role in the cardio-renal axis, mediating adverse outcomes.
Despite strengths, including matching and comprehensive biomarker assessment, limitations include the observational design that cannot confirm causality and a single timepoint biomarker measurement at admission. The cohort’s age and comorbidity profiles also warrant cautious generalization to younger or less sick populations.
Mechanistically, proteins like IGFBP-7 and TIMP-2 are involved in cell cycle arrest and tubular stress responses, while MCP-1 and CCL-14 reflect inflammatory chemokine activity, linking kidney injury to systemic inflammation and heart failure pathophysiology.
Future studies should explore whether interventions targeting tubular injury pathways can improve outcomes and if serial biomarker monitoring enhances risk prediction.
Conclusion
This study highlights the clinical relevance of kidney tubular biomarkers in patients hospitalized with acute heart failure. Biomarkers such as IGFBP-7, KIM-1, MCP-1, and CCL-14 identify patients at increased risk for death and heart failure readmission independent of glomerular function and cardiac biomarkers. Incorporating tubular health measures into clinical practice may enhance risk stratification and enable more personalized care for acute HF.
Emerging kidney tubular biomarkers thus represent promising tools for refining prognosis and guiding therapeutic strategies in this high-risk patient group. Ongoing research is needed to validate their utility and integrate them into clinical guidelines.
References
Wettersten N, Duff S, Horiuchi Y, et al. Kidney Tubular Biomarkers Predict Risk of Death and Heart Failure Readmission in Acute Heart Failure. J Am Heart Assoc. 2025 Sep 5:e042880. doi:10.1161/JAHA.125.042880. Epub ahead of print. PMID: 40913274.
Bellomo R, Kellum JA, Ronco C. Acute kidney injury. Lancet. 2012;380(9843):756-766.
Damman K, Testani JM. The kidney in heart failure: an update. Eur Heart J. 2015;36(23):1437-1444.
Mishra J, Ma Q, Prada A, et al. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol. 2003;14(10):2534-2543.