Highlights
- AUN, a combination of two natural bacteria, achieves complete tumor clearance in mouse and human cancer models—even in severely immunocompromised hosts.
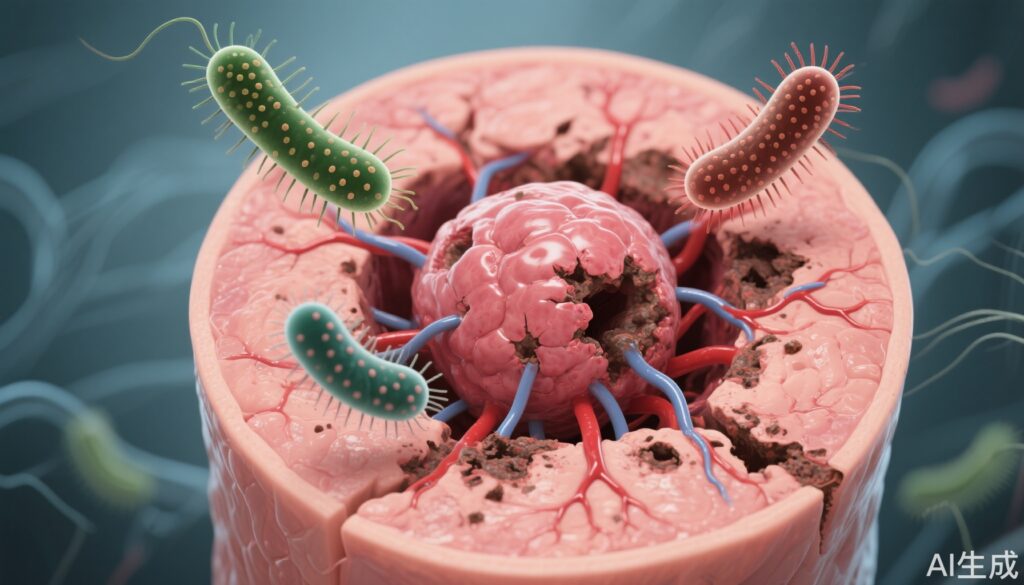
- This bacterial therapy induces selective thrombosis and necrosis within tumors, independent of host immune cells.
- Structural transformation of tumor-resident bacteria and dramatic microbiome shifts underlie the potent, targeted antitumor effects.
- AUN demonstrates high biosafety, minimal side effects, and potential applicability across diverse cancer types.
Study Background and Disease Burden
Cancer remains a leading cause of morbidity and mortality worldwide. While immunotherapies such as checkpoint inhibitors and CAR-T cells have transformed cancer care, their efficacy depends heavily on the patient’s own immune system. Many patients, particularly those who have undergone extensive chemotherapy or radiotherapy, are left immunosuppressed and cannot benefit from these approaches. Historically, bacterial infection has been observed to trigger tumor regression, dating back to Busch’s 1868 report and Coley’s toxins in the late 19th century. However, safe and effective translation of bacterial therapy to the clinic has been elusive, largely due to safety concerns and lack of precise tumor targeting. The recently published study by Iwata et al. (Nat. Biomed. Eng 2025) introduces a paradigm-shifting approach: a microbial consortium (AUN) that eradicates tumors independent of the host immune response.
Study Design
The AUN microbial therapy is composed of two naturally occurring bacterial strains: Proteus mirabilis (A-gyo), a tumor-resident species, and Rhodopseudomonas palustris (UN-gyo), a photosynthetic bacterium. In preclinical experiments, AUN was administered intratumorally or systemically to various mouse models, including those with severely compromised immune systems (nude, SCID, and NOD-SCID mice). Tumor types included colon (Colon26), human colorectal cancer (HT29), ovarian (SKOV3), and pancreatic (BxPC3) cell-derived tumors. Key endpoints were tumor regression, survival, safety (body weight, systemic toxicity), and mechanistic biomarkers (histopathology, cytokine profiles, tumor microenvironment changes).
Key Findings
AUN therapy achieved remarkable antitumor activity in all evaluated models:
– In immunodeficient mice (nude, SCID, NOD-SCID), AUN led to complete regression of established tumors, with 100% remission in optimal dosing schedules (initial low dose followed by high dose).
– Tumors treated with AUN exhibited rapid darkening within 24 hours, attributable to selective, intratumoral thrombosis and vascular collapse. This was confirmed by marked increases in coagulation factor VII activity and the presence of extensive fibrin deposition.
– Histological analyses (H&E, TUNEL, TNF-α staining) revealed massive tumor cell apoptosis, fragmentation, and a robust local inflammatory response—despite the absence of functional immune cells in the host.
– Mechanistically, A-gyo transformed from short swimmer cells (~2.5 μm) to long swarmers (20–50 μm) exclusively in the presence of tumor metabolites (fumarate, lactate, O-phosphoethanolamine, spermidine), allowing deep penetration into tumor cores. This transformation did not occur in the presence of normal cells, highlighting strong tumor selectivity.
– The intratumoral bacterial ratio shifted dramatically from the initial 3:97 (A-gyo:UN-gyo) to 99:1 within the tumor microenvironment, a key factor in reactivating suppressed hemolytic and oncolytic activities.
– UN-gyo acted as a regulator, suppressing the pathogenicity of A-gyo while enhancing tumor-specific cytotoxicity. The AUN consortium did not cause hemolysis in human blood or release pro-coagulant factors, underlining its safety profile.
– AUN upregulated genes involved in extracellular iron acquisition. Since tumors are highly dependent on iron for growth and metastasis, this iron depletion may contribute to the observed tumor suppression.
– High-dose single injections occasionally led to cytokine release syndrome (CRS), but this was preventable with pre-treatment using heparin (anticoagulant) or dexamethasone (anti-inflammatory steroid), demonstrating that safety can be managed via dosing strategies.
– Across multiple human cancer models in immunosuppressed mice, AUN treatment resulted in complete tumor disappearance without intolerable side effects.
Expert Commentary
The AUN bacterial consortium represents a significant advance in microbial cancer therapy. Its unique mechanism—precise vascular targeting, structural bacterial transformation, and dynamic population shifts—enables effective tumor killing without reliance on the patient’s immune system. This is especially promising for patients who are ineligible for current immunotherapies due to immune exhaustion or suppression.
Importantly, the use of non-genetically engineered, naturally occurring bacteria minimizes regulatory and safety hurdles compared to synthetic or recombinant strains. The dual-bacterial approach also offers a built-in safety mechanism, as UN-gyo tempers the pathogenicity of A-gyo and prevents systemic toxicity.
Limitations include the need for further validation in larger animal models and, ultimately, humans. While safety in mice is encouraging, monitoring for unexpected off-target effects or sepsis in humans will be critical. Additionally, the requirement for intratumoral or systemic injection may limit use for certain tumor locations, and long-term effects remain to be established.
Conclusion
The preclinical success of the AUN bacterial consortium introduces a new era of immune-independent bacterial oncology. Its robust efficacy, safety profile, and broad applicability could reshape the therapeutic landscape for difficult-to-treat cancers, particularly in immunodeficient populations. Further research is warranted to translate these findings into clinical trials and assess their impact on human cancer care.
References
1. Iwata, S., Nishiyama, T., Sakari, M. et al. Tumour-resident oncolytic bacteria trigger potent anticancer effects through selective intratumoural thrombosis and necrosis. Nat. Biomed. Eng (2025). https://doi.org/10.1038/s41551-025-01459-9
2. Coley, W.B. The treatment of malignant tumors by repeated inoculations of erysipelas. With a report of ten original cases. Am J Med Sci. 1893.
3. Busch, W. Über die Entwicklung von Krebs nach Verletzungen. Berliner klinische Wochenschrift, 1868.