Highlights
- Standalone safety planning interventions did not significantly reduce suicide ideation, attempts, or healthcare re-presentations among adolescents.
- Current evidence is limited by moderate to high risk of bias and small sample sizes.
- The utility of safety planning as an adjunct to other interventions remains to be determined.
- More rigorous, large-scale studies are urgently needed to guide adolescent suicide prevention strategies.
Study Background and Disease Burden
Suicide is among the leading causes of death for adolescents globally, with rates of suicidal ideation, attempts, and hospitalizations rising over the past decade. The burden is particularly acute as adolescence is a period of heightened psychosocial vulnerability. While safety planning interventions (SPIs)—a structured, collaborative approach to identifying coping strategies and sources of support during crisis—are recommended and effective in adults at high risk for suicide, the evidence base for their use in pediatric populations is much less robust. Given the increasing prevalence and severity of suicide-related behaviors in youth, there is a critical need to clarify the effectiveness of SPIs for adolescents and inform best practices in clinical settings.
Study Design
This systematic review and meta-analysis by Albaum et al. (JAMA Pediatr. 2025) aimed to evaluate the effectiveness of safety planning as a standalone intervention for adolescents with suicidal ideation or suicide-related behavior. The authors searched Ovid MEDLINE, OVID PsycINFO, EBSCO CINAHL, and Scopus (Elsevier) for studies published between January 1, 2008, and March 26, 2024. Eligible studies included peer-reviewed research (with or without a control condition) assessing SPI in adolescents, with outcomes of suicidal ideation, suicide-related behaviors (including attempts), and re-presentations to healthcare settings (e.g., emergency department visits or hospital admissions). Nonempirical studies, gray literature, and non-English publications were excluded. Data extraction and quality appraisal were performed independently by two reviewers, employing random-effects meta-analytic models and the Joanna Briggs Institute Critical Appraisal tools.
Key Findings
Ten studies with a combined sample of 1002 adolescents (mean age 15.0 years; 76% female) met the inclusion criteria. Of these, five studies (n=619) provided sufficient data for meta-analysis. The principal findings were as follows:
– **Suicidal Ideation:** No significant association was found between SPIs and reductions in suicidal ideation at follow-up (Hedges g = 0.11; 95% CI, 0.01-0.21). The observed effect size was small and not clinically meaningful.
– **Suicide-Related Behavior:** No significant effect was identified for suicide-related behaviors, including attempts (Hedges g = -0.09; 95% CI, -0.20 to 0.02), or for actual suicide attempts (Risk Ratio [RR], 1.03; 95% CI, 0.12-8.88).
– **Healthcare Re-Presentation:** No significant effect of SPI was found on re-presentations to healthcare settings for suicide-related reasons (RR, 0.99; 95% CI, 0.29-3.35).
Figure 2. Forest Plots of the Association Between Safety Planning Interventions (SPIs) and Suicide-Related Outcomes.
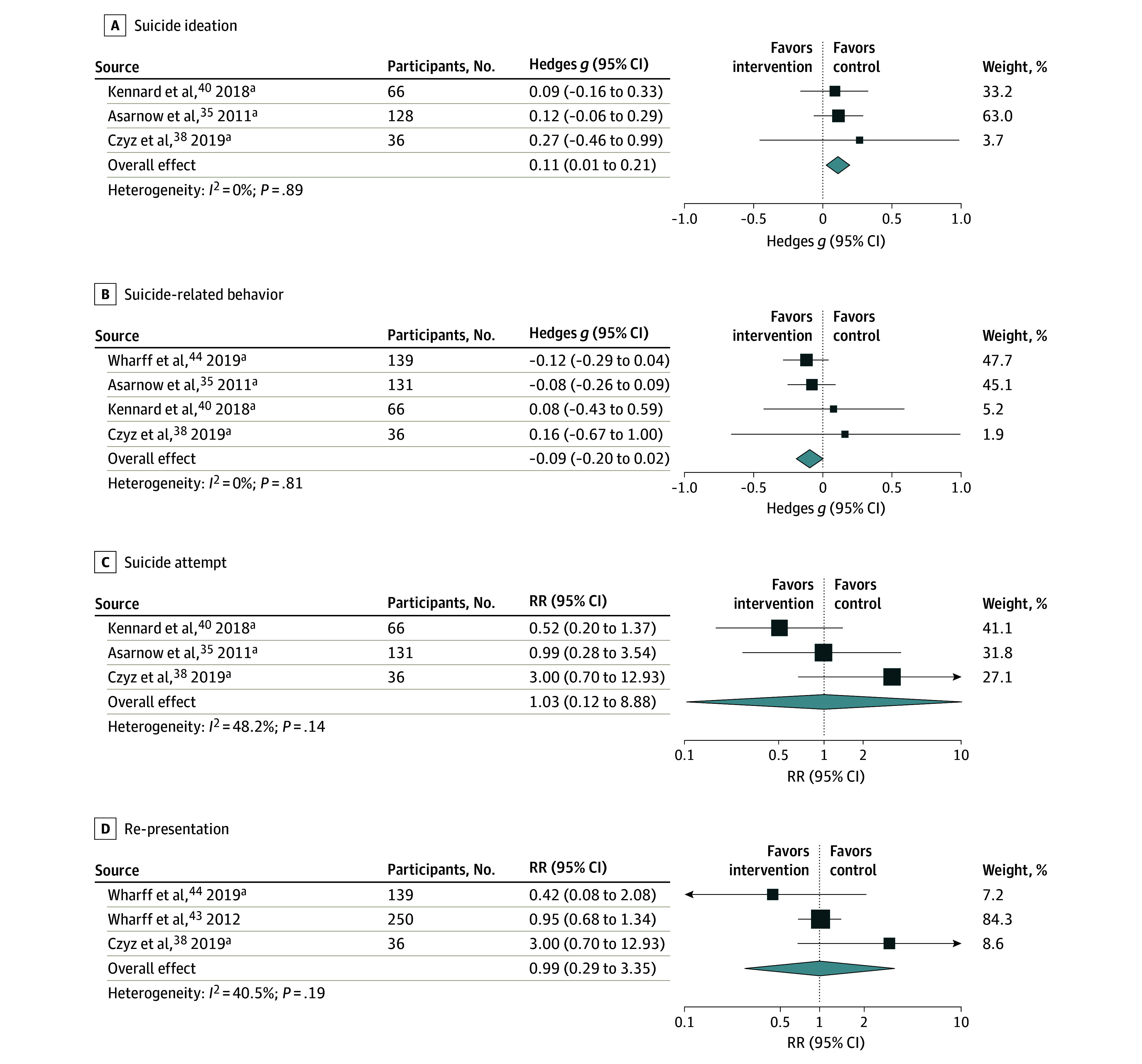
Notably, heterogeneity was moderate to high across studies, and risk of bias was assessed as moderate to high for the majority of included studies, primarily due to methodological limitations, lack of blinding, and small sample sizes. The lack of significant findings persisted across sensitivity analyses and was not explained by differences in follow-up duration, intervention fidelity, or population characteristics.
A summary of pooled effect sizes is presented below:
| Outcome | Effect Size (Hedges g/RR) | 95% CI | Significance |
|——————————|—————————|——————|———————|
| Suicidal Ideation | 0.11 | 0.01 – 0.21 | Not significant |
| Suicide-Related Behavior | -0.09 | -0.20 – 0.02 | Not significant |
| Suicide Attempts (RR) | 1.03 | 0.12 – 8.88 | Not significant |
| Healthcare Re-presentation | 0.99 | 0.29 – 3.35 | Not significant |
Expert Commentary
The findings of this meta-analysis highlight a critical evidence gap in adolescent suicide prevention. While safety planning is a pragmatic, widely implemented strategy in clinical practice, its efficacy as a standalone intervention for adolescents remains unproven. Experts in adolescent psychiatry and suicide prevention note several key considerations:
– **Complexity of Adolescent Psychopathology:** Adolescents frequently present with comorbidities (e.g., depression, substance use, trauma) and complex psychosocial stressors, which may limit the standalone effectiveness of brief interventions like SPI.
– **Implementation Fidelity:** Variability in how SPIs are delivered, the degree of family and caregiver involvement, and follow-up support may influence outcomes, yet these factors were often inadequately reported.
– **Adjunctive Role:** Current clinical guidelines recommend SPIs as part of a broader multimodal approach, including psychotherapy (such as cognitive-behavioral or dialectical behavior therapy), pharmacotherapy when indicated, and family interventions. The limited effect of SPI alone does not negate its potential utility as an adjunct to comprehensive care.
– **Research Gaps:** The field urgently requires well-powered randomized controlled trials with clear reporting of intervention components, adherence, and long-term outcomes. Moreover, research should assess whether certain subgroups (e.g., those with prior attempts, high-risk psychiatric profiles) might derive more benefit from SPI.
Conclusion
This systematic review and meta-analysis underscore the paucity of high-quality evidence for the effectiveness of standalone safety planning interventions in adolescents at risk for suicide. Current data do not support the use of safety planning alone to reduce suicidal ideation, attempts, or suicide-related healthcare utilization in this population. Until further robust evidence emerges, safety planning should be considered as one component of a comprehensive, individualized, and multidisciplinary approach to adolescent suicide prevention. Clinicians are encouraged to integrate SPIs with evidence-based psychotherapies and family engagement and to closely monitor at-risk youth during transitions in care.
References
1. Albaum C, Irwin SH, Muha J, Schumacher A, Clarissa S, Finkelstein Y, Bridge JA, Korczak DJ. Safety Planning Interventions for Suicide Prevention in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2025 Aug 1;179(8):886-895. doi: 10.1001/jamapediatrics.2025.1012 IF: 18.0 Q1 . PMID: 40388177 IF: 18.0 Q1 ; PMCID: PMC12090068 IF: 18.0 Q1 .2. Stanley B, Brown GK. Safety planning intervention: A brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19(2):256-264.3. Brent DA, Melhem N. Familial transmission of suicidal behavior. Psychiatr Clin North Am. 2008;31(2):157-177.4. Horowitz LM, Bridge JA, Teach SJ, et al. Ask Suicide-Screening Questions (ASQ): A brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med. 2012;166(12):1170-1176.


