Highlights
- Early DOAC restart after major bleeding in AF patients does not significantly reduce stroke but increases recurrent bleeding risk.
- The benefit in stroke reduction is marginal and not statistically robust.
- Optimal timing for DOAC resumption remains unresolved, underscoring the need for individualized approaches.
- Current evidence supports further randomized trials to define best practices.
Clinical Background and Disease Burden
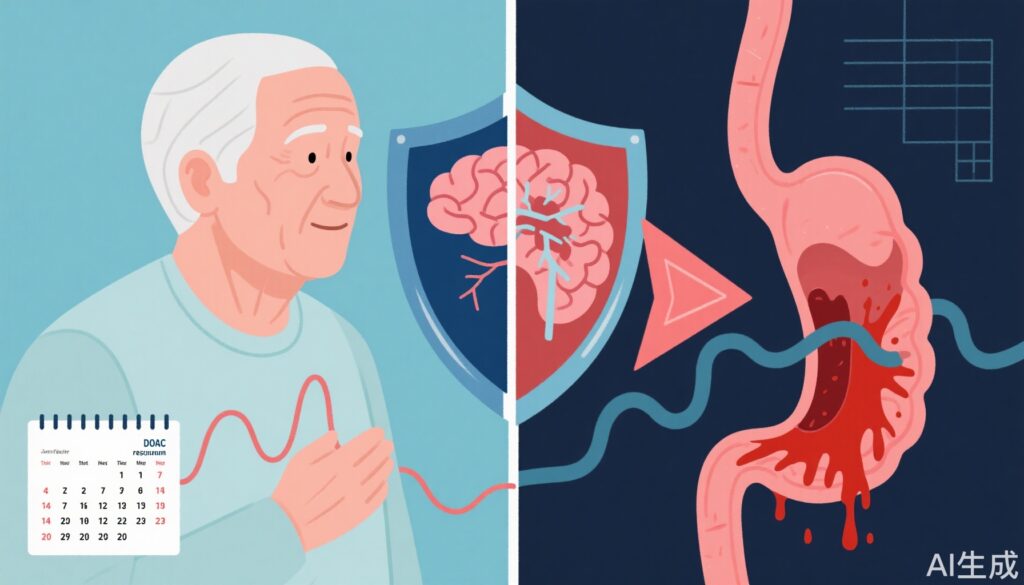
Atrial fibrillation (AF) is a prevalent cardiac arrhythmia associated with a substantial risk of ischemic stroke. Direct oral anticoagulants (DOACs) are cornerstone therapies for stroke prevention in AF, offering advantages over vitamin K antagonists, such as fewer dietary restrictions and predictable pharmacokinetics. However, the major adverse effect of DOACs remains serious bleeding, which complicates management and raises questions about the optimal timing for resumption post-bleeding. Clinicians must navigate the delicate balance between mitigating thromboembolic risk and avoiding recurrent hemorrhagic events—a dilemma intensified by limited high-quality evidence.
Research Methodology
The referenced study by Al-Hussainy et al. utilized a nationwide Danish registry from 2012 to 2021 to identify AF patients (CHA₂DS₂-VASc score ≥2) who experienced their first serious bleeding event while on DOAC therapy. Patients were stratified by the timing of DOAC resumption: those restarting within 60 days (early restarters) vs. those resuming after 60 days (late restarters). Multivariable Cox proportional hazards models were used to calculate hazard ratios (HRs) for stroke, recurrent bleeding, and a composite endpoint (stroke or serious bleeding). Secondary analyses explored six time-varying antithrombotic regimens.
Key Findings
Of 10,291 patients surviving 60 days post-bleed, 5,970 restarted DOACs early and 4,321 later. Key findings include:
- Stroke Risk: During one-year follow-up, 242 early restarters and 194 late restarters experienced a stroke (event rates: 4.7 vs. 5.2 per 100 patient-years). The adjusted HR for stroke in early vs. late restarters was 0.89 (95% CI 0.74-1.08), suggesting a non-significant trend toward benefit.
- Recurrent Bleeding: Serious bleeding occurred in 752 early and 451 late restarters (15.4 vs. 12.8 per 100 patient-years). Early restart conferred a higher risk of recurrent bleeding, adjusted HR 1.21 (95% CI 1.07-1.36).
- Composite Endpoint (Stroke/TIA/Bleeding): Events occurred in 954 early and 609 late restarters (20.0 vs. 17.6 per 100 patient-years), with an adjusted HR of 1.13 (95% CI 1.02-1.26), mainly driven by recurrent bleeding.
- Sensitivity Analysis: Changing the early restart cut-off from 60 to 30 days nullified differences in recurrent bleeding and composite endpoint risks, indicating timing nuances.
A summary table is presented below for clarity:
| Outcome | Early Restarters (per 100 pt-yrs) | Late Restarters (per 100 pt-yrs) | Adjusted HR (95% CI) |
|---|---|---|---|
| Stroke | 4.7 | 5.2 | 0.89 (0.74–1.08) |
| Recurrent Bleeding | 15.4 | 12.8 | 1.21 (1.07–1.36) |
| Composite Event | 20.0 | 17.6 | 1.13 (1.02–1.26) |
Mechanistic Insights and Biological Plausibility
The observed increased risk of recurrent bleeding with early DOAC resumption is biologically plausible, as the healing of vascular endothelium post-hemorrhage may be incomplete, predisposing to rebleeding. Conversely, prolonged interruption of anticoagulation increases the risk of thromboembolism, particularly in high CHA₂DS₂-VASc score patients. The lack of significant stroke reduction with early restart likely reflects a complex interplay between underlying patient risk, event timing, and competing mortality risks.
Expert Commentary
Current guideline recommendations, such as the 2020 European Society of Cardiology (ESC) guidelines, acknowledge the lack of definitive evidence for optimal timing of anticoagulation resumption after major bleeding. Leading experts advocate individualized clinical decision-making, incorporating patient comorbidities, bleeding site, risk scores (CHA₂DS₂-VASc, HAS-BLED), and patient preferences. Dr. Gregory Y.H. Lip, a co-author of the study, has previously emphasized the importance of balancing thrombotic and bleeding risks and the need for further randomized data.
Controversies and Study Limitations
This observational study, while robust in sample size and national coverage, is subject to several limitations:
- Potential for residual confounding and selection bias, despite multivariable adjustments.
- Lack of granular data on bleeding severity, heparin bridging, and investigations during anticoagulation interruption.
- Exclusion of patients who died or had events within the first 60 days post-bleed limits generalizability.
- Findings are associative, not causative.
These limitations underscore the need for randomized controlled trials on this topic, though such trials face practical and ethical challenges.
Conclusion
Restarting DOACs early after a serious bleeding event in AF patients offers only marginal reduction in stroke risk at the cost of increased recurrent bleeding. The findings reinforce the importance of individualized risk assessment and shared decision-making. Until randomized trial data become available, clinicians should carefully weigh the risks and benefits in partnership with patients, considering the timing, nature of bleeding, and overall thromboembolic risk.
References
- Al-Hussainy N, Kragholm K, Lundbye-Christensen S, Torp-Pedersen C, Pareek M, Krohn Therkelsen S, Lip GYH, Riahi S. Timing of anticoagulation restart after serious bleeding in atrial fibrillation. Heart. 2025 Jul 16:heartjnl-2024-325343. doi: 10.1136/heartjnl-2024-325343 IF: 4.4 Q1 .
- Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation. Eur Heart J. 2021;42(5):373–498.
- Steffel J, Collins R, Antz M, et al. 2021 European Heart Rhythm Association (EHRA) practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Europace. 2021;23(10):1612–1676.